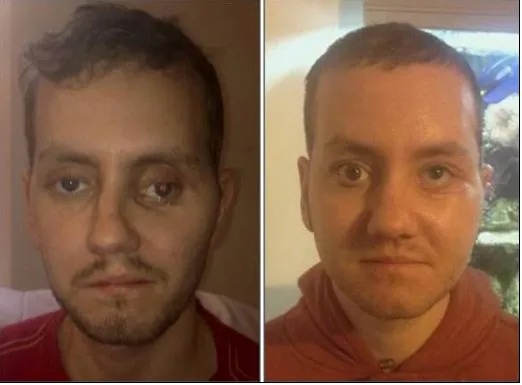
How 3D Printing Helped Repair This Man’s Face
In a landmark procedure, surgeons used 3D printing techniques to restore a patient’s facial likeness after a horrific injury
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/79/b8/79b81718-d4e8-4542-a978-06e37b6e4f4b/theatre.jpg)
News coverage of advances in 3D printing tends to play up fun applications of the technology—musical instruments, fashionable clothes and tasty treats—or ideas that stretch the imagination, like 3D printed houses and cars.
While it might not be as flashy, additive manufacturing has been quietly revolutionizing the medical field, and the lives of patients with debilitating conditions. Its most recent champion: Stephen Power, a 29-year-old man from Wales who has a new face thanks to an innovative surgical technique that incorporates 3D scanning and printing.
In 2012, Power had a horrific motorcyle accident. Though he was wearing a helmet, the impact fractured his upper jaw, cheek bones, nose and skull. Power was rushed to Morriston Hospital in Swansea for a series of emergency procedures that managed to repair most—but not all—of his injuries.
"We fixed his facial fractures pretty well but he had damaged his left eye and the ophthalmologists did not want us to do anything that might damage his sight further," Adrian Sugar, a maxillofacial surgeon, said in a press release. "So the result was that his cheekbone was too far out and his eye was sunk in and dropped."
It would be several months before doctors began planning reconstructive surgery to restore symmetry to Power's face. Using the conventional process, a surgeon would typically practice on a rough model of a patient's face built from off-the-shelf parts. Surprisingly, the process is as inexact as it sounds, with the specialist mapping out each step using what Sean Peel, a prosthetics designer at the National Centre for Product Design and Development Research (PDR) at Cardiff Metropolitan University, describes as "visual judgments and crude measurements.”
Peel and Sugar, along with other researchers, decided instead to pursue a different approach—one they hoped could correct the damage to Power's face with more precision.
Thanks to a collaboration between Morriston Hospital and Cardiff Metropolitan University, a 3D scan of Power's face was used to design cutting guides and plates to help the surgeons map where features like cheekbones should be placed. Using all of that data, the team printed the guides, plates and medical-grade titanium implants, which doctors used to ultimately reconstruct Power's face.
Though 3D printed implants have been used in surgery before, the doctors say this is the first time the technology has been employed in each phase of the process.
"The advantage with 3D printing is that the information and subsequent parts helps the surgeon achieve superior accuracy, predictability and a reduction in operation time," Peel says. "It is much more accurate than relying on visual judgments in surgery, and the improved predictability allows the operating team to anticipate any problems that might arise during the procedure or even mitigate them well before the procedure takes place."
With the improved accuracy, patients can avoid the potential cost of follow-up procedures; less time on the operating table also allows patients to recover faster and lowers the risk of infection, he adds.
During Power's eight-hour operation, Sugar used the custom-printed tools to re-fracture Power's cheekbones. He repositioned the fragments to match specs generated by the computer model. The implants were then inserted to hold the bones in place as well as raise his eye to its original position.

“Without this advanced technology, it's freehand," Sugar explained in a statement. "You have to guess where everything goes. The technology allows us to be far more precise and get a better result for the patient.”
After the surgery, doctors noted that Power's left eye is still slightly raised, though they expect it to settle over the next few months.
"It is totally life-changing," Power told the BBC. "I could see the difference straightaway the day I woke up from the surgery."
So far, the surgery has a good track record in the United Kingdom. But the team doesn't know enough about things like the optimal design process or workflow to regularly implement the technology on a routine basis—yet. A larger research initiative is expected to yield answers that could make the procedure a possibility for patients worldwide.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/tuan-nguyen.jpg)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/tuan-nguyen.jpg)