This Smartphone Microscope Uses Video to Spot Moving Parasites
A team of Berkeley bioengineers has created CellScope, a mobile phone attachment that can quickly test blood for tropical diseases
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/2b/59/2b59db03-8673-4d30-afa4-ee5a4431ea2f/loa-outdoors.jpg)
Smartphones can take your pulse, monitor your mental health, keep track of your diet, analyze your sleep cycle and help control your diabetes. Now, a new smartphone technology can spot parasites in your blood, in a fraction of the time it would take a laboratory technician.
Developed by a team at the University of California at Berkeley, CellScope is a smartphone microscope that uses video to detect parasite movement. It is currently being tested for use in diagnosing two neglected tropical diseases endemic in parts of the developing world, onchocerciasis and lymphatic filariasis. If widely adopted, it could vastly improve treatment in places where people often lack access to basic medical services.
“The idea of using mobile phones for microscopy is something we’ve been working on for a number of years, starting way back when cameras started appearing on phones,” says Daniel Fletcher, a professor of bioengineering at Berkeley, who heads the lab that created CellScope. “We were convinced early on that these devices could be developed into a range of different applications.”
To understand what makes CellScope unique, you need to understand how onchocerciasis and lymphatic filariasis work.
A bite from a female blackfly can transmit onchocerciasis, or river blindness, while mosquitoes spread lymphatic filariasis, or elephantiasis. In both diseases, the insects deposit larvae, which then take up residence in the human body and grow into worms. Symptoms of onchocerciasis include skin nodules, terrible itching (sometimes so bad people will burn their skin to stop it), and, in some cases, vision loss. It is the second leading cause of infectious blindness in the world. Lymphatic filariasis causes thickening of the skin and swelling of limbs, which can be severe.
Fortunately, an antiparasitic drug called ivermectin can be used to treat onchocerciasis and lymphatic filariasis. But here’s the catch: many people with these two diseases are also infected with Loa loa, another parasite. Give ivermectin to someone with a Loa loa infection, and the patient can suffer severe side effects and even die. Testing for Loa loa is time-consuming though and takes scientific equipment and expertise.
The “gold standard” of Loa loa diagnosis has always been the blood smear, says Fletcher. This is where a blood sample is placed on a glass slide, treated with a stain and observed under a microscope. Depending on how far the patient is from a laboratory facility, getting results can take days.
“In order to rapidly diagnose a vast number of people we needed something much faster,” Fletcher says.
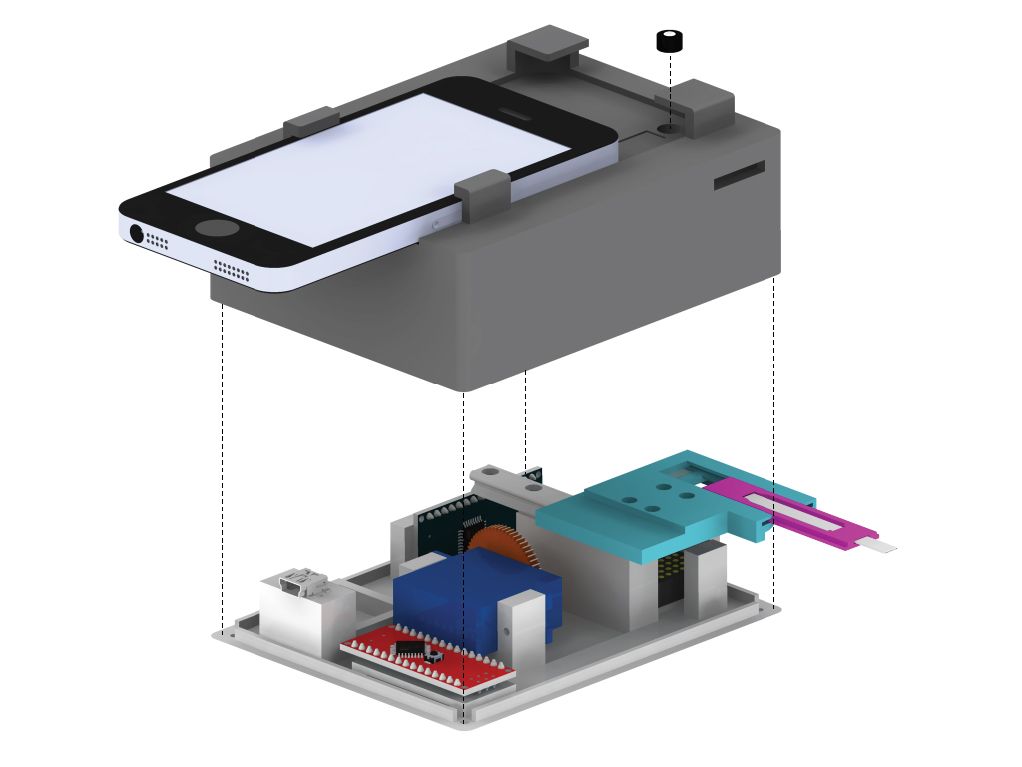
Eventually, the team hit on the idea of using the worms’ movement to detect them automatically. CellScope works like this: a mobile phone sits on top of a 3D printed base with a slot for a blood sample. The base includes LED lights, microcontrollers and a USB port. When the blood sample is inserted, the phone communicates with the base to take a series of videos. Then, an algorithm looks for the motion of the Loa loa worms in the video. Results are available almost instantly. If there’s no Loa loa infection, the patient can start ivermectin right away.
Unlike traditional Loa loa diagnosis, which requires a lab and a trained technician, CellScope can be used by anyone, anywhere. This is especially important in places like rural Cameroon, where a team of researchers collaborating with Berkeley has been doing ongoing testing of CellScope and there can be little access to conventional medical care. Its automation also reduces human error, a common issue in lab diagnostics.
Fletcher hopes CellScope will be useful in diagnosing other parasites, such as soil-transmitted helminths (a category which includes roundworm, hookworm and whipworm) and trypanosomes, which cause sleeping sickness and Chagas disease. CellScope could also be a useful tool for diagnosing non-parasitic diseases, such as tuberculosis in places where traditional microscopes are few and far between.
The next step for CellScope is a larger study involving some 40,000 subjects in Cameroon. In addition, two former students of Fletcher’s have founded a startup called CellScope to bring products based on the CellScope technology to market.
“Our hope is that this combination of hardware and software automation that’s all driven by these powerful mobile phones is going to provide a solution for those diseases,” he says.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/matchar.png)

/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/matchar.png)