Why Black Lung Disease Is Deadlier Than Ever Before
As President Trump prepares to send miners back to work, a near-obsolete illness is once again ravaging coal country
:focal(980x428:981x429)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/df/11/df115d90-4346-4d0b-b544-380245cf7ab0/gettyimages-168796579.jpg)
Update, February 8, 2017: Since this story was written, NIOSH has published new results in the Journal of the American Medical Association documenting the largest cluster yet of advanced black lung cases. In just three clinics that treat miners in Virginia, Kentucky and West Virginia, 416 new cases of black lung were reported.
William McCool was always a stickler for safety.
A 63-year-old retired miner from Kentucky, McCool wore his protective dust mask any time he descended into the underground tunnels. From his first day on the job in 1973 at Volunteer Coal Company in Tennessee to the day he left the mines in 2012, he would affix the mask firmly to his face—just as his father, who was a miner before him, had done.
Though many of his coworkers complained that the masks were clumsy to breathe through, McCool never questioned its importance. Every night, he would hand the mask to his wife, Taffie. And every night for 40 years, she would wash the mask clean, placing it in his dinner bucket for him to take to work the following day.
His precautions weren't enough. In 2012, McCool was diagnosed with advanced black lung. "We thought we were protecting our lungs," he says now. "[But] you can’t see the dust that really hurts you."
Black lung is the common term for several respiratory diseases that share a single cause: breathing in coal mine dust. McCool has the classic form of the disease, coal worker’s pneumoconiosis. Over time, his lungs had become coated in the same black particulates that he’d tried to protect himself against all those years. Their delicate passageways had become etched in dark scars and hard nodules.
These diseases are progressive, and they have no cure. More than 76,000 miners have died of black lung since 1968, according to statistics from the U.S. Department of Labor. These include several of McCool’s friends from the mines, who died in their 60s. One friend has been put on a list to receive a lung transplant, which is considered a last-resort treatment. Even if he gets one, it will likely only increase his lifespan by three to four years. “If I live to be 66 or 68, that’s a long time,” says McCool.
After every other sentence, he coughs—a dry, hollow sound—to clear his lungs.

Last month, President Trump visited the Washington, D.C., headquarters of the Environmental Protection Agency to approve an executive order that would reduce regulatory burdens on the coal and oil industries. Surrounded by coal miners from Rosebud Mining Company, he sat down to sign the Executive Order on Promoting Energy Independence and Economic Growth. “You know what it says, right?” he asked the miners. “You’re going back to work—that’s what it says.”
As many news outlets were swift to report, it’s not at all clear that the order will actually resurrect mining jobs in a declining industry. With increasing mine automation, competition from cheap natural gas, and technological advances driving down the cost of renewable energy, there is simply less demand for the product that sends people like McCool underground. But what is certain is that coal mining is still far from a safe job—and in recent decades, the work has become increasingly dangerous for long-term miner health.
On-the-job mine safety has improved drastically in recent decades, with deaths due to accidents now counted in the tens, not hundreds, as they were in the 1970s and 80s. Long-term health, however, is a different story. As the administration seeks to fulfill the campaign promise to send miners in coal country back to work, black lung has made a comeback. Today, the disease sickens roughly 1 in 14 underground miners with more than 25 years experience who submit to voluntary check ups—a rate nearly double that from the disease’s lowest point from 1995 to 1999.
Even more worrisome, the disease is striking miners earlier and in a more deadly form than ever before. Though experts are still working out the causes for the rise in disease, many believe it is a combination of both longer hours on the job and new methods of rock extraction. In the wake of Trump’s executive order, we asked legal and health experts: Just how dangerous are the jobs we could be sending miners back to?
The term “black lung” sounds downright archaic. The name brings to mind a sickness that struck down populations long before modern medicine had taken shape—like typhoid, the plague, or the Black Death. Yet in the last several years, black lung has mysteriously rebounded in central Appalachia, where coal is still king—namely in Kentucky, Virginia and West Virginia.
“Most of us studied these diseases in medical school, but were under the impression that they were relics of a bygone age,” writes Robert Cohen, a pulmonologist at the University of Illinois who specializes in black lung, in an editorial for the British Medical Journal last year. “We believed that modern mining technologies and dust controls, which have been in place for decades, had eliminated this scourge. We were wrong.”
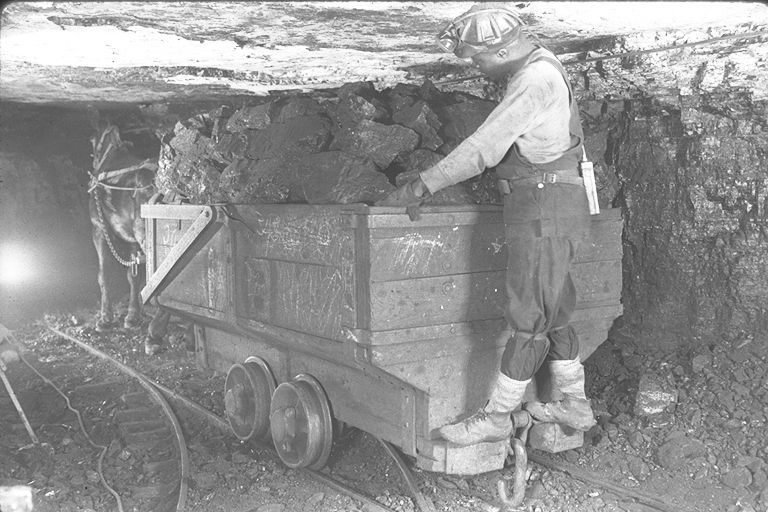
Indeed, reported cases of black lung had been on decline since the passage of the Coal Mine Health and Safety Act in 1969, the first comprehensive mine safety legislation. That bill almost didn’t pass. Spurred on by union groups including the United Mine Workers of America, it was introduced in the Senate after a massive mine explosion killed 78 miners in Farmington, West Virginia in 1968. President Richard Nixon hesitated to approve the legislation due to concerns over how worker’s compensation would be doled out.
The final persuading factor may have been a visit Nixon received by seven widows of miners who had died in the blast. He refused to see the women, but within 24 hours, he had signed the bill into law.
The act not only reduced on-the-job tragedies, it also marked a pivotal moment in the history of long-term miner health. The law established the agency that would eventually become the Mine Safety and Health Administration (MSHA), which would hold companies accountable for the removal of dangerous dust from the mines—venting the tunnels, partitioning sections with curtains, and tamping down dust with streams of water that prevents dust clouds from whipping up in the wake of large machinery.
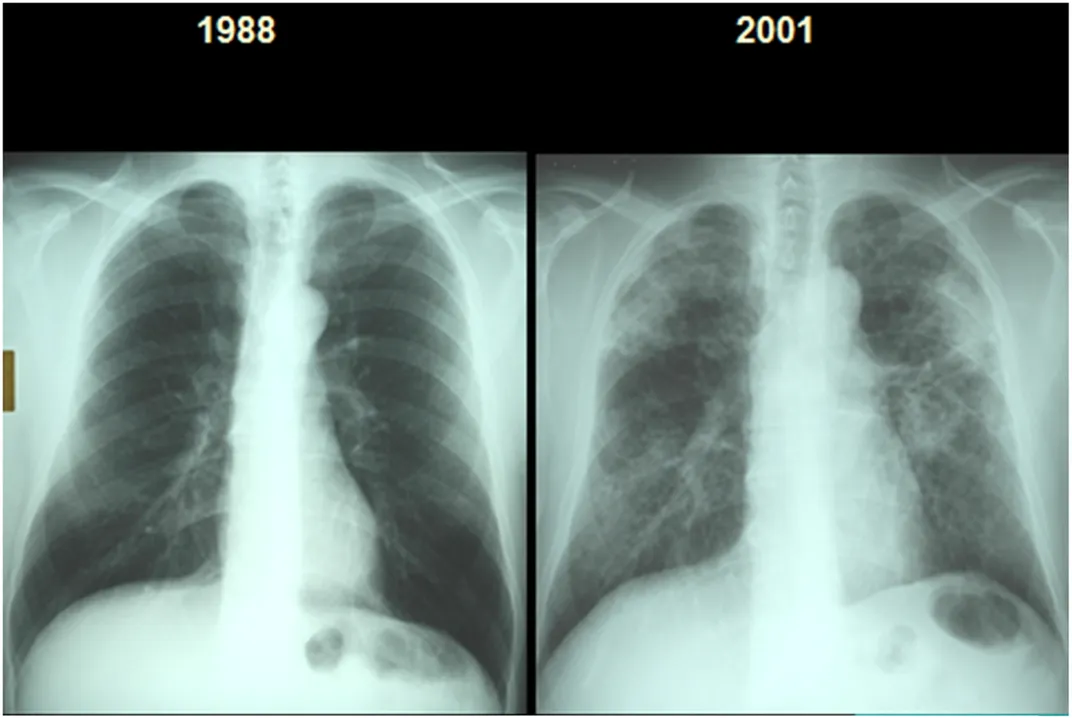
By the late 1900s, black lung had reached an all-time low, with only 31 cases of the worst form of the disease reported from 1990 to 1999. Most experts considered it nearly obsolete.
The first signs of a rebound in black lung diagnoses came in the early 2000s, says Cohen. These weren’t your “typical,” run-of-the-mill cases. “Instead of this very slow, gradual, insidious process, we were seeing miners whose lungs were getting scarred up much more quickly,” Cohen says. Many developed into the worst form of the disease: progressive massive fibrosis, or PMF, characterized by large masses of scar tissue and nodules.
Wes Addington, who works with miners filing for black lung benefits as deputy director at the Appalachian Citizens’ Law Center, confirms this trend. Until recently, it was rare for him to see a PMF case, but in the last five or six years he estimates the number has increased tenfold. “It’s unbelievable how many of those cases I’m getting,” he says.
In 2016, the National Institute for Occupational Safety and Health (NIOSH) documented 60 cases of PMF in just 20 months at a single small health clinic in Kentucky. They published their findings a report in the Morbidity and Mortality Weekly.
At the same time, NPR was conducting an extensive investigation into the extent of the disease. Reporters collected records from 11 black lung clinics in Virginia, West Virginia, Pennsylvania and Ohio. They found a stunning 962 cases so far this decade—more than double the 441 cases NIOSH had documented in the last 40 years. “The true number is probably even higher,” wrote investigative reporter Howard Berkes. “[S]ome clinics had incomplete records and others declined to provide data.”
“The sad part is it is all preventable,” says Addington, who has represented McCool in his ongoing fight for black lung benefits. “This is a disease of the early 20th century not the early 21st century.”
So why is it still happening? And why is it striking miners earlier—and more intensely—than ever before?
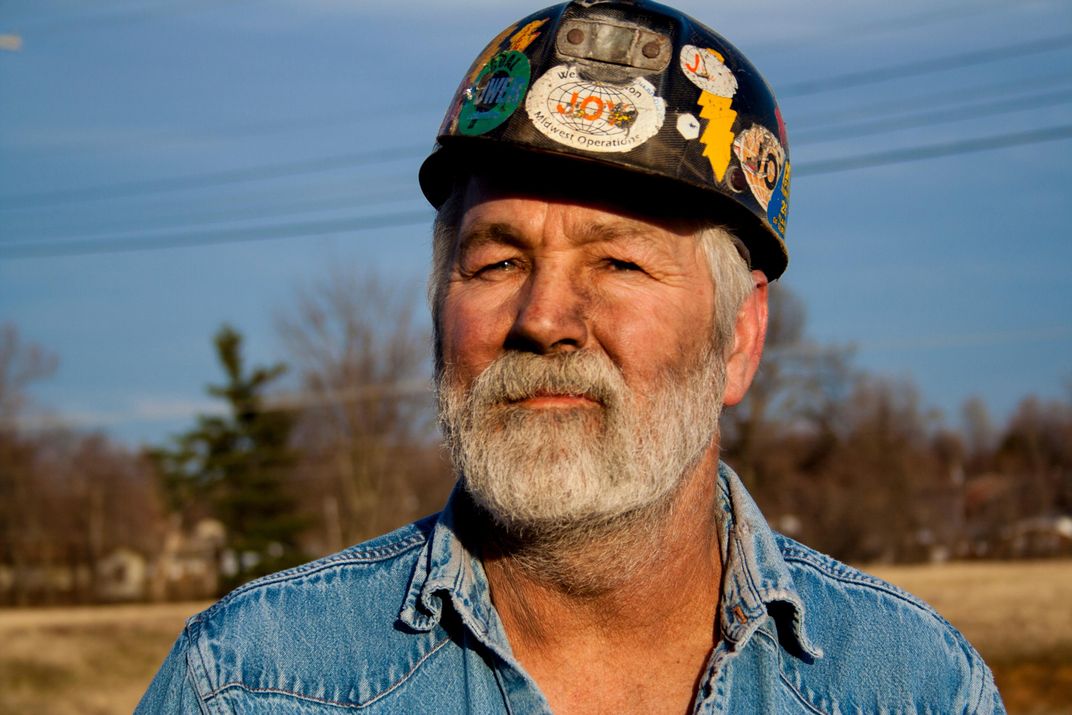
Michael “Flip” Wilson had a very different journey into coal than McCool. The first coal miner in his family, Wilson entered the mines when he was 18 years old. It was 1974, and he was seeking his fortune in what was then a booming industry in Kentucky.
Wilson spent 41 years toiling down dark, winding tunnels in search of coal seams—layers of valuable fuel sandwiched between rock. For most of that time he operated what’s known as the “continuous miner,” a machine that carves away the mine’s walls and breaks apart massive seams into bite-sized hunks. Unlike McCool, however, he rarely used a facemask.
The masks were burdensome, he says. Dust would collect over the filters, clogging them up and requiring frequent changes. “You just couldn’t breathe through them,” he says. So Wilson foraged ahead with the continuous miner, clouds of inky black dust billowing in its wake.
Three years ago, Wilson was diagnosed with black lung. Not using a facemask may certainly be one way that coal dust found its way into his lungs. But Wilson is also among a new generation of miners working without the safety net of mine unionization, which research suggests helps protect workers from unsafe conditions and company dishonesty.
Miners at non-union mines often don't report safety violations for fear of losing their jobs, Addington explains. Dust, in particular, has faded to the background. “Miners are more likely to put up with excessive dust because it doesn’t threaten them and the bigger stir that they cause the more likely they are to lose their job,” says Addington, who also files lawsuits against companies for unjust treatment of workers who speak up. “It’s much more difficult for miners to complain about excessive dust than other safety and heath issues at a coal mine.”
“I always did what the coal company wanted me to do, if it was right or if it was wrong,” Wilson recalls. “I should have known better, but at the time I needed the job.”
Armstrong Coal did not respond to repeated requests for comment.
Unions became popular among miners during the late 1800s, with today’s largest organization, the United Mine Workers of America (UMWA), founded in 1890. The UMWA has been instrumental in improving conditions for miners, from shorter work hours to safer working conditions. It was also a driving force in drawing attention to the issue of respiratory disease during the early 1900s, a time when “strenuous denial of the existence or extent” of black lung was still rampant, according to a 1991 article in the American Journal of Public Health.
Measuring the effects these unions have had on overall mine safety has been difficult, in part due to confounding factors like mine size and the fact that unionized mines tend to report more injuries than non-unionized ones. But a Stanford Law School study published in the journal Industrial and Labor Relations Review in 2013 found that unionization had resulted in a “substantial and significant decline” in both fatalities and traumatic injuries.
Today, however, mine unions have declined along with mining jobs. Union representation has fallen by over 50 percent in the last decades—from 14 percent in 1997 to just 6 percent in 2016. In Kentucky, where some of the highest rates of black lung are being reported, the last unionized mine shuttered its doors in 2015.
Experts reason that longer work days may also contribute to the current surge in black lung. Fewer breaks give workers less time to flush their lungs with clean air, says Cohen, which can rid their lungs of particulate that has not yet taken root. Wilson estimates that he worked an average of 70 to 80 hours per week while at Armstrong Coal. “A lot of the time I would come in on day shift,” he says. “I worked 10 [or] 11 hours that day, then I would go home and sleep three or four hours. And then I'll go back on third shift.”
There’s yet another reason for the rise. Many researchers believe the disease’s new intensity stems in part from the size of the coal seams being mined. These days, coal companies have plundered most of the thick seams of pure coal and now seek thinner and thinner veins. That means miners are taking out more rock along with the coal using heavy machinery. As a result, the clouds of black dust have grown increasingly muddled with silica, a much more potent lung irritant.
Coal mine dust isn’t just coal; it’s a mix of coal, silica and other elements like iron. Silica’s toxicity comes from a variety of chemical properties, including electrostatic charge—the same force that makes your hair stand on end when rubbed with a balloon—and what is known as “reactive oxygen species” (ROS). When these highly reactive particles make their way deep into the respiratory system, they can lance the lung cells, resulting in a flood of damaging enzymes that harm the tissue.
Dust from coal, silica and iron are all thought to contain ROS on their surface, says Cohen. But studies suggest that silica—especially freshly ground or cut silica—is especially reactive. Cohen and his colleagues are currently studying the toxicity of this dust by examining the material found in the lungs of black lung sufferers in different stages of the disease. He believes this toxicity is a key to figure out why some people develop classic pneumoconiosis, while others go on to get PMF.
Understanding that, however, requires knowing how this devastating disease takes hold in the first place.

From the hairs in your nose to dust-catching mucus in your throat, your body is equipped with safeguards to protect the delicate tissues of your lungs. But the tiniest dust particles can slip by these defenses undetected. The smaller the dust, the deeper it can go, and the more damage it can inflict.
To make the trip down your throat and into your respiratory system, the dust must be less than five microns across—just smaller than the diameter of a red blood cell. Coal mine dust is rife with these tiny particles. “It's not something our defenses were evolved to handle,” says Cohen.
It’s impossible to say exactly why McCool, who wore his mask every day, got black lung. While there are some respirators that can filter out these tiny particles, they have to be properly fit and sealed to the face at all times, explains Cohen. Oftentimes, these just aren’t practical underground. “I've never met a miner that used a mask all the time,” he says. “You can't cough you can't spit … you can't really do heavy labor pulling air through a mask.”
For those like Wilson who don’t wear the masks, and even for some like McCool that do, the dust gets into the lungs. And once it’s in, it doesn’t come out. Instead, it triggers the immune system, provoking a cascade of responses aimed at attacking and killing what is recognized as a foreign invader. But because the invader is a mineral—which, unlike viruses or bacteria, can’t be easily broken down—that system can rapidly be overwhelmed.
When this happens, the immune system cells explode. They send out chemical calls for help, essentially flashing red alerts in the body. The inflammation and barrage of killer enzymes that ensues does little to repel the intruding dust. Instead, the lungs become casualties of battle, pierced through by the released chemicals and enzymes. Particles that are potentially toxic themselves—including coal, iron and silica—only worsen the damage.
As they work to repair themselves, the lungs form scar tissue and the nodules characteristic of black lung. Over time, the black particulate coats them, turning them as black as coal—hence the name.
Victims of black lung often suffer bouts of coughing that produce copious amounts of dark, inky phlegm. In 1881, one doctor highlighted this viscerally by using the jet-black fluid that one of his patients had coughed up to jot down a note for a medical conference. “The sentence I am reading was written with this fluid,” he is reported to have told his audience. “The pen used has never been in ink.”
The classic form of black lung, which McCool suffers from, is known as coal worker’s pneumoconiosis, a condition characterized by small nodules less than one centimeter in diameter. In recent years, doctors have learned that the dust can cause a range of other chronic obstructive airway diseases, including bronchitis and emphysema. In the latter, the lung begins digesting itself, until it’s riddled with holes.
Black lung ultimately leaves its victims gasping for every breath. “You’d do anything to get some air,” says McCool. Before he got on oxygen, he had what he called “breathing attacks,” which he says feel similar to panic attacks. Once, McCool had an attack so severe that he got out of bed and headed outside, thinking it would be easier to breathe in the fresh night air. But he found no relief. “It didn’t help,” he says.
With few treatments available, prevention is the only way to save miners from this fate. Inhalers can help treat the symptoms of black lung, and oxygen can help the miners breathe. There are no long-term solutions other than lung transplants; a recent study suggests that the transplant only grants an average of some 3.7 years more of life.
Wilson, who was featured in a Huffington Post profile last year. is still in the early stages of his disease. His condition has worsened since 2012, and doctors predict his lungs will continue to degrade. He currently uses an inhaler to help him breathe, but he says he can’t afford the oxygen that would soothe the cough that flares at night. When asked how he planned to address his disease’s progression, he laughed drily.
“There ain't no cure for it,” he said. “It’s just like a cancer. It just keeps eating.”
On paper, regulations for dust levels in the mines have been steadily improving. In 2014, the Mine Safety and Health Administration passed new regulations—the third and final stage of which became active last year—setting some of the lowest dust limits found anywhere in the world. The new regulations also “plugged up” loopholes for dust sampling that had been abused for decades, says Cohen.
One of the major loopholes has to do with dust pumps, the devices used to measure the levels of dust in any given mine. Until recently, the devices collected samples of dust from the air on filters, which were then sent out to labs for analysis.
But these were easily thwarted, Wilson recalls. “They would give [the dust pump] to me and an hour later they would take it and hang it in fresh air,” says Wilson about his supervisors at Armstrong Coal. “I was told to put it in my dinner bucket; I was told to wrap a rag around it.” He recalls once being instructed to “do whatever [you] have to do to make the dust pump come in [clean].”
Since the new regulations, companies are required to use pumps that measure dust levels in real-time, and aren’t as easily thwarted. Due to the disease’s slow progression, it will take at least a decade before researchers see whether these new rules have had any effect. In the meantime, many challenges still stand in the way of these regulations being effective.
For one, many miners decline to undergo the free examinations that federal regulations entitle them to every five years, says Anita Wolfe, program coordinator for the coal workers health surveillance program administered through NIOSH. Some are afraid of losing their jobs or other forms of company retaliation, several miners told Smithsonian.com. Wolfe says that oftentimes a miner won’t get examined until after he or she retires, by which point the disease could have progressed.
"Some miners just flat out don't want to know if they're sick or not … they're going to continue to work. That's their livelihood," she says. She estimates current participation in screening programs is about 40 percent overall, but in states like Kentucky, it’s as low as 17 percent.
Second, miners aren’t always made aware of the risks. This is particularly common among surface miners, who weren’t considered at risk for black lung until recently. In one of NIOSH’s outreach trips to Oklahoma, Texas and Louisana, Wolfe was surprised at how little the miners knew about the disease. “When you talk to those miners about black lung, they look at you like you’re speaking a foreign language,” she said in a 2015 presentation.
Yet the risks are real, says a miner from Armstrong Coal who wishes to remain anonymous due to fear of industry retaliation. “A lot of people don’t understand it, don’t believe it. But it is real.” All the miners Smithsonian.com spoke with recounted the many friends and coworkers either already dead or currently dying from the disease—some as young as 29.
So along with MSHA’s new dust regulations, NIOSH has been working to catch more cases of black lung in a timelier manner. In doing so, they hope to better understand the explosion of cases and to help miners whose lungs have succumbed to disease exit the mines sooner.
In 2006, NIOSH launched their Enhanced Coal Workers Surveillance Program, in which “a mobile examination unit”—i.e. a van loaded with lab equipment—travels across the country to provide easier access to the screenings. There, medical professionals not only take detailed work histories and blood pressure, but also do a chest X-ray and breathing test. (In 2008, the organization also released a video featuring two miners with black lung to help spread awareness about the disease.)
This is often one of the only times the miners see a doctor, says Wolfe. It’s not just that they fear getting a diagnosis of black lung, she says, describing the miners as a “hardy bunch,” who don’t readily consult doctors. The problem also goes back to miners’ taxing schedules: “Most of the miners tell us they just don’t have the time,” she says.

Nearly all of the experts who spoke to Smithsonian.com agreed on one thing: Periods with the fewest cases of black lung are the result of strong mine regulation and enforcement of those regulations. And the future of miner’s health and safety relies on keeping mine operations in check.
MSHA’s recent dust regulations and NIOSH’s continued outreach and education efforts are a start, says Cohen. Simply creating these safety measures, however, isn’t enough to guarantee their success. “With an appropriate investment in dust controls and stuff, it can be made safer,” he says, adding, “it does take money, and it does take investment. If you're not going to do that, then it's not going to be safe.”
Though NIOSH hopes to continue with its mobile screening units, “there’s always concern about funding when you're running a federal program,” says Wolfe. The black lung surveillance is mandated by Congress, but the lab-on-wheels is not part of that mandate. Traditional clinics are also in need: While funding for the clinics has remained steady for years, Cohen says more is needed to address the recent surge in cases.
“A lot of these guys are now out, no jobs, and for the first time, many of them are actually thinking about what happened to their lungs,” says Cohen. “We're now overwhelmed with large numbers of these cases.”
For those who already have the disease and have already left the industry—like McCool and Wilson—the path isn’t easy. For those who can still work, very few jobs await in the heart of coal country. "For decades it’s been the only game in town," says Addington. For those who can’t and are seeking black lung benefits, it’s a rocky road ahead. “Miners need help,” says McCool. “It’s too late for a lot of them, but for the ones that's in bad shape, they need to be took care of.”
Though McCool is completely debilitated from his disease, his benefits claim has been pending for five years. While he waits, he’s living off of short-term state benefits. “But in 2020, that’s over with,” he says. He pauses, then adds: “If I make it that long.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Wei-Haas_Maya_Headshot-v2.png)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Wei-Haas_Maya_Headshot-v2.png)