Can Saving Animals Prevent the Next Deadly Pandemic?
A global disease monitoring network is banking on the idea that healthier wildlife means healthier humans
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/33/75/33756874-b0b8-4123-bfbd-74d9fdc9a3ce/bats.jpg)
In the fall of 2014, the deadly Ebola virus jumped from an unknown animal to a 2-year-old boy in Guinea. The virus quickly spread to others around him and began terrorizing West African nations; by April 2016, more than 11,000 people had died. Researchers now believe that fruit bats were the origin of this zoonotic disease—which refers to any disease that makes the jump from animals to humans (or vice versa), and includes around 75 percent of all emerging infectious diseases.
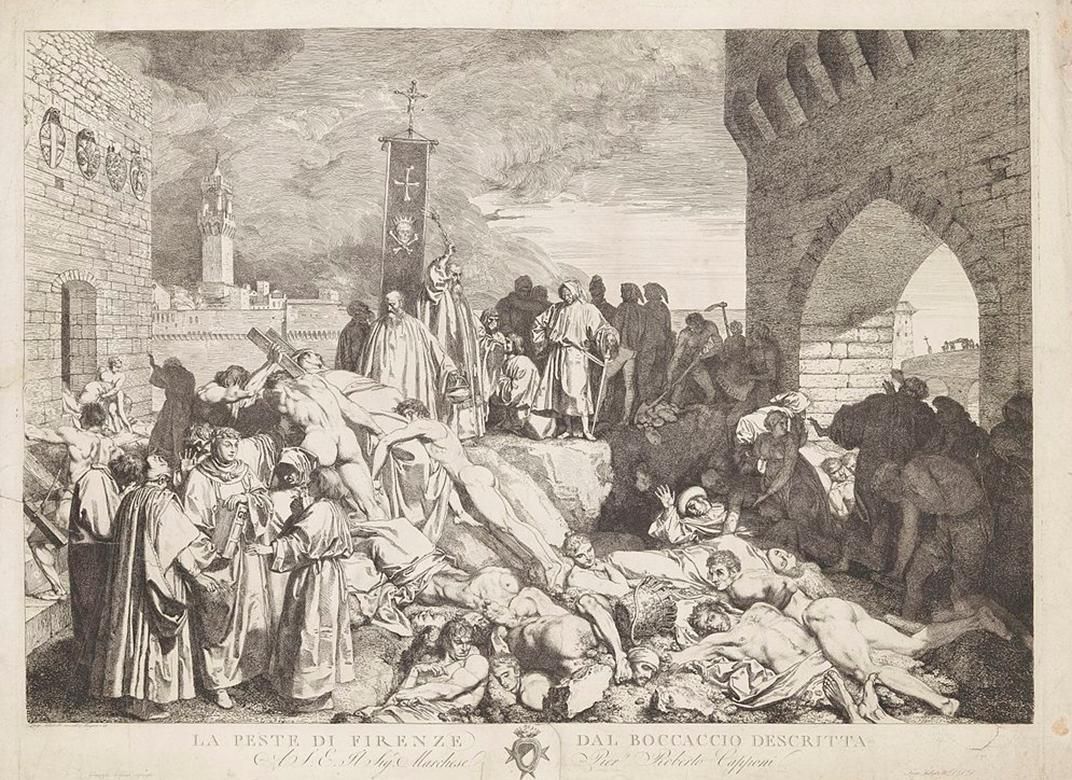
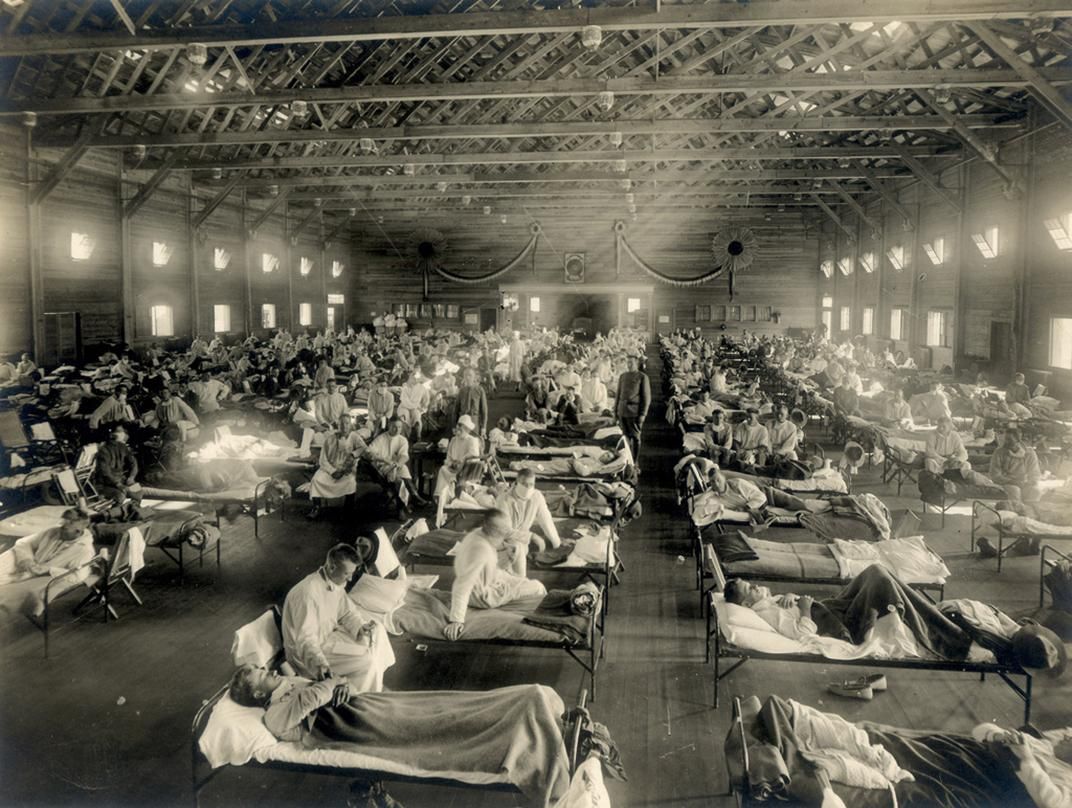
Zoonotic diseases are at the root of some the world’s worst pandemics. Bubonic plague, for instance, originated in city rats, and was usually transferred to humans via an infected flea bite. HIV/AIDS started as a virus in Old World monkeys in Africa. The more recent swine flu, while less fatal, has been traced back to pigs raised for food in North America. The Spanish Influenza of 1918 has been traced back to birds and killed around 50 million people, more than twice as many as were killed in World War I.
Not all of these species-jumping sicknesses are viruses. Bubonic plague stems from a bacterial infection, and malaria, which may have killed as many as half of all humans who have ever lived, is a parasite transmitted by mosquitoes. But there’s a reason viruses are the inspiration behind classic pandemic horror stories like World War Z or Contagion.
“Many of the bacterial or fungal or parasitic diseases that humans get from animals are harder to transmit between people,” says Kali Holder, a wildlife pathologist and Morris Animal Foundation Global Health Fellow at Smithsonian. “Viruses mutate so much faster than anything else, and because many are easily transmitted, what you have is a perfect storm.”
Yet the Ebola outbreak, bad as it was, could have been much worse. In August of that same year, another scare quietly took place in the Équateur Province of the Democratic Republic of the Congo. But in that case, just 49 people died, and the World Health Organization declared the end of the outbreak within three months. This remarkable success was thanks to fast action by local governments, medical partners and a relatively new global disease surveillance network known as USAID PREDICT.
Now eight years old, USAID PREDICT is a collaborative effort to monitor, predict and prevent emerging diseases, many of them zoonotic, from becoming devastating global pandemics the likes of Ebola. It’s led by Jonna Mazet, an epidemiologist at the University of California at Davis’s One Health Institute and School of Veterinary Medicine, and also partners with the Wildlife Conservation Society, Metabiota, EcoHealth Alliance and the Smithsonian Institution’s Global Health Program.
In the case of Ebola in 2014, PREDICT had done extensive advance work in the DRC, training local researchers in safe sampling techniques and setting up a regional network to respond quickly to zoonotic diseases like Ebola. That work is a big part of why most people never heard of that second Ebola outbreak.
In its first five years, PREDICT trained 2,500 government and medical personnel in 20 countries on things like the identification of zoonotic diseases and implementing effective reporting systems. They collected samples from 56,340 wild animals, using innovative techniques like leaving chew ropes for monkeys then collecting saliva afterwards. They also detected 815 novel viruses—more than all the viruses previously recognized in mammals by the International Committee on Taxonomy of Viruses.
Part of the way PREDICT prevents outbreaks is by monitoring diseases in animals, in the hopes of keeping viruses from crossing over to humans. So far the group has provided support during 23 outbreaks and four wildlife epidemics; it also creates vaccines for domestic livestock like poultry. This is all part of the “one health” theory that undergirds the program: When wildlife and ecosystems are healthy, and diseases are diluted, humans are healthier, too.
Which means that the immediate goal of human health comes with a nice side effect: wildlife conservation.
“When you disrupt an ecosystem by removing a species through culling, you have a less healthy ecosystem and higher risk of disease,” says Megan Vodzak, a research specialist for Smithsonian’s Global Health Program. “Sometimes you increase the level of the virus within the population because you eliminate some but not all of the animals, and they’re still circulating it.”
This is known as the dilution effect, which hypothesizes that a higher rate of species richness creates a buffer against zoonotic pathogens.
In her pathology work for Smithsonian’s Global Health Program, Holder has done everything from develop safer protocols for collecting samples from bats—“they’re amazing transmitters of disease, so we [have to find] how much we can detect without putting our grubby little paws on a grubby little bat”—to identifying a pathogen causing oozing skin lesions in rhinos (it turned out to be a nematode worm).
While this work undoubtedly helps the animals suffering from these pathogens, it could also have benefits for humans. “Not only are we responding to save ecosystems and endangered animals, we’re also the first line of defense with regards to identifying potential zoonotic diseases,” Holder says.
Even though the animals at the National Zoo aren’t exposed to most of the diseases wild populations contract, scientists can use the captive species to learn about treatment. One recent example is using long-lasting antibiotics in giant pandas. “Now that we know they can maintain levels for over 10 days, that changes how we would treat an animal in the wild,” says Suzan Murray, director of the Global Health Program. Smithsonian virologists, pathologists, anesthesiologists and wildlife veterinarians who can identify diseases in lions and elephants and rhinos all contribute their knowledge and expertise to the program.
For those who value both conservation and human health, the idea that protecting wildlife can also mean preventing epidemics is a welcome one. But, like most conservation challenges in world shaped by humans, it’s not always that simple. A recent study published in the journal Philosophical Transactions of the Royal Society B found no significant human health benefit from increasing biodiversity. The researchers surveyed biodiversity and infectious diseases around the world for 20 years (they used forestation as a proxy for biodiversity, since there are no reliable counts of species going back 20 years).
Although this study looked at 24 known diseases rather than emerging pandemic threats, the lessons may still be applicable when it comes to conservation. “Results from our analysis indicate as you increase forest, you can exacerbate the number of diseases transmitted,” says Chelsea Wood, one of the study’s authors and a conservation ecologist at the University of Washington. “That’s a message I hesitate to deliver as a conservationist, but it’s what the data show.”
Wood became skeptical of the dilution effect when she did comparative studies of islands being fished versus un-fished. What she found was that certain parasites actually disappeared in the presence of fishing, and flourished in the more “pristine” environment. She found another example in onchocerciasis, a disease transmitted by a parasitic worm in East Africa known more commonly as “river blindness.”
Since a drug was invented to treat river blindness in the 1970s, the disease has declined dramatically. But another reason for the decline, Wood points out, is regional deforestation. River blindness is transmitted by black flies that breed on the backs of crustaceans that live in shadowy freshwater rivers. As shade cover from trees decreased due to deforestation, the prevalence of the disease-transmitting flies lessened as well.
“I know that conservation provides so many benefits to human society beyond infectious disease transmission,” Wood says. “But [with dilution theory] we consistently find a mixed bag, which is not a good outcome for people interested in selling conservation as disease control.”
Again, Wood emphasized that her findings apply to known diseases, not future possible pandemics we have yet to identify. But when researchers do embark on conservation projects, she cautions that they should also consider other possible outcomes besides the protective benefit humans get from healthy wildlife and ecosystems. “We have to recognize that conservation could provide benefits for public health and it could endanger public health," she says.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/lorraine.png)

/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/lorraine.png)