Doctors Use a Dissolvable 3D-Printed Tracheal Splint to Save a
An infant’s collapsing airway now has a device holding it open; as his tissue strengthens, the splint will be absorbed into his body
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/20130522040159splint-small.jpg)
For most of human history, any baby who suffered a collapsed trachea or bronchi faced a tragic fate: suffocation. These tubes convey air from the mouth to the lungs, and some infants are born with congenitally weakened cartilage surrounding them, a condition known as tracheomalacia. In severe cases, this can lead the trachea or bronchi to collapse completely, blocking the flow or air and causing a newborn to suddenly stop breathing.
To the amazingly wide-ranging list of accomplishments attributed to 3D printing technology, we can now add one more: a custom-made tracheal splint that saved the life of an infant with tracheomalacia and will be safely absorbed into his tissue over the next two years. A team of doctors and engineers from the University of Michigan printed the splint and implanted it into six-week-old Kaiba Gionfriddo last year, and announced the feat in a letter published today in the New England Journal of Medicine.
In December of 2011, Giondriddo was born with tracheomalacia, a condition that affects roughly 1 in 2200 American babies. Typically, the weakened cartilage causes some difficulty breathing, but children grow out of it by age 2 or 3 as the trachea naturally strengthens over time. His case, though, was particularly severe, and in February 2012, his parents April and Bryan were out to dinner when they noticed that he suddenly stopped breathing and was turning blue.
He was rushed to a hospital and kept alive with a ventilator, but doctors said there was a good chance he wouldn’t be able to survive long-term. Several weeks later, a team of Michigan engineers led by Scott Hollister began designing the device, based off prior research, in which they’d 3D printed splints and other prostheses but hadn’t implanted them in clinical patients. For this splint, they used a CT scan of Giondriddo’s trachea and left bronchus to create a 3D digital representation that was then printed, allowing them to produce a splint that would perfectly match his airway’s size and contours.

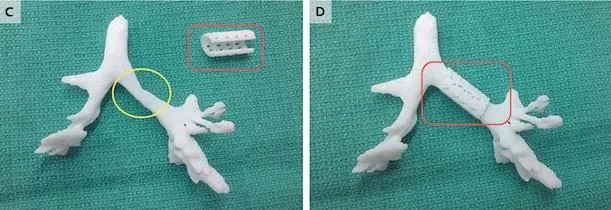
On February 21, 2012, the splint was surgically sewn around Giondriddo’s failed bronchus; almost immediately, it held open his air passages and allowed him to breathe normally. “It was amazing. As soon as the splint was put in, the lungs started going up and down for the first time,” Glenn Green, the doctor who performed the surgery and helped design the splint, said in a press statement.
21 days later, Giondriddo was taken off the ventilator and has had no breathing problems in the 14 months since the surgery. In addition to holding open the bronchus, the splint also provides a skeleton upon which natural cartilage tissue can grow, and because it was printed using a biopolymer called polycaprolactone, it will gradually be absorbed into this body tissue over time.
Previously, severe tracheomalacia was treated by extended periods of time using a ventilator, or the implantation of mesh tubes around the trachea or bronchus to keep the airway open. By custom-designing the splint based off a CT scan, though, the team created a treatment method that they say is more effective. Additionally, the dissolvable material means Giondriddo won’t need invasive surgery later to remove the device.
The team has also worked on using this same CT scanning and 3D printing process to produce custom-made ear, nose, skull and bone prostheses that are currently in experimental phases. Other research groups have successfully implanted 3D printed ears, noses and skulls in clinical patients, while last month, an Oxford team figured out how to print microscopic droplets that behave like human tissue.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/joseph-stromberg-240.jpg)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/joseph-stromberg-240.jpg)