America’s Long-Overdue Opioid Revolution Is Finally Here
Thanks to advances in neuroscience, researchers are beginning to disentangle powerful pain relief from addiction, overdose and death
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/53/5c/535c024f-e293-4abd-a53c-5b54d8ed74f8/gd894t.jpg)
A bunion, you may have the misfortune to know, is a bony growth that forms at the base of your big toe. When that bump begins to irritate the rest of your foot, it has to go.
Wincing would be the correct reaction here. On the pain scale, a bunionectomy doesn’t compare to having a limb sawn off; nor is it particularly medically risky. But since it “involves shaving off extra bone and cutting the big toe in half and pinning it back together,” says David Soergel, chief medical officer of the pharmaceutical company Trevena Inc, “it’s actually a very painful surgery.” That wince-worthy quality makes it the perfect surgery on which to test cutting-edge new pain relievers—such as Oliceridine, Trevena’s newest and most promising opioid compound.
For more than 200 years, doctors have soothed their patients’ pain with morphine, the drug isolated from the opium poppy and named after Morpheus, Greek god of dreams. And morphine has generally lived up to its reputation as an effective painkiller. But because of how it works on the central nervous system, morphine also has a host of notorious side effects, from nausea to life-threatening respiratory depression to addiction. So in 2014, Soergel and his team were on the hunt for a safer—and more effective—painkiller. The hope was that Oliceridine could provide equal or better pain relief than morphine, while reducing those nasty side effects.
In the trial, 330 bunionectomy patients received either Oliceridine, morphine or a placebo after their surgery. Those that received either drug reported pain relief within minutes (as opposed to hours for the poor souls who had only been given the placebo). But while patients given 4 mg of morphine reported that it took about a half hour for them to feel any relief, those given 4 mg of Oliceridine reported an average of just two minutes. Oliceridine, which was designed to take advantage of researchers’ new understanding of the underlying neuroscience of opioids, ultimately proved to be about three times as potent a painkiller as morphine. Even better, peer-reviewed studies showed that it was far less likely to cause dangerous side effects.
The result “could be a substantial advance in opioid pharmacotherapy,” Soergel and his colleagues reported in the journal PAIN in June of that year. They expanded on the drug's potential in the abstract of another study, presented in October 2016 at the annual meeting of American Society of Anesthesiologists. "This novel mechanism of action could lead to ... rapid, effective analgesia with improved safety and tolerability,” the team wrote.
Today, Oliceridine is the only opioid compound of its kind to be tested on humans. It’s now in Phase III clinical trials, with results due in early 2017; if all goes well, it could be brought to market within the next few years, according to Trevena co-founder Jonathan Violin. The drug’s potential is great. Oliceridine—and other compounds like it—could be just the first of a host of medicines with all the powerful pain relief of morphine, but far fewer devastating side effects. And they’ve all been made possible by our new understanding of the neuroscience behind these compounds. “This could be the first in what you might think of as a new class of opioids,” says Violin.
And the truth is, it’s about time.

A Revolution on Hold
There are few elements of medicine that haven’t progressed since the 19th century. Today, physicians work in antiseptic operating rooms and wield antibiotics to fight infection, rather than bone saws for the removal of gangrenous limbs. Modern anesthesia is a sophisticated medical concoction, compared to chloroform on a rag or a shot of whiskey. But when it comes to treating severe pain, we still rely on the same go-to substance we’ve been using since at least 3400 B.C.E: opium.
There’s a reason we’ve been so loyal to this flower: It works. Since antiquity, humans have utilized the power of the opium poppy to ease pain, treat disease and generate euphoria. The Sumerian civilization knew the poppy as hul gil, or “plant of joy” more than 5,000 years ago; there are visual hints of the poppy in Greek artifacts stretching back to 1500 B.C.E. Roman physicians in the first and second centuries C.E. recommended opium mixed with wine prior to the amputation of limbs. In 1784, British surgeon James Moore recorded the first known use of opium to ease pain after surgery.
In 1805, German pharmacist Friedrich Serturner changed the game by isolating morphine from opium. Other developments in that century would expand on that success, improving the delivery and distillation of this potent compound. In the 1850s, the development of the hypodermic syringe allowed exact dosages of morphine to be delivered directly into a patient’s bloodstream, which would be key for field hospital amputations during the American Civil War. In the 1890s, morphine was expanded into an array of morphine-like medications known collectively as the opioids.
Taken together, this suite of medications—which are today available as pills, injections, lollipops and patches—has revolutionized the treatment of pain. But the relief they bring is not without cost. Morphine would also prove to have a dark side. Even in the 19th century, addiction among soldiers was reportedly prevalent enough to earn the moniker “the soldier’s disease.”
Today, morphine addiction is America’s disease. In the U.S., the overprescription and abuse of opioid medications has led to a growing addiction crisis. Since 1999, the number of fatal opioid overdoses in the U.S. have quadrupled. So have the number of prescriptions written for opioid pain medications. According to Debra Houry, director of the National Center for Injury Prevention and Control at the CDC, 249 million opioid prescriptions were written in 2013—enough for every American adult to have their own bottle. And many who become addicted to these medications move on to a cheaper and more dangerous black market drug: heroin.
In the 1890s, Bayer pharmaceuticals began marketing heroin—which is made by applying the chemical process of acetylation to morphine—as a supposedly more potent and less addictive alternative to morphine. Heroin would prove to be about two to four times more potent than morphine, but claims that it was less addictive would prove unfounded in dramatic fashion. In 2015, the American Society of Addiction Medicine estimated almost 600,000 Americans were addicted to heroin. According to the Surgeon General’s report on addiction released in November, more than 28,000 Americans died from the use of prescription opioids or heroin in 2014.
What can be done about this epidemic of highly addictive, often fatal pain-killers? The obvious answer, you might think, would be to ditch opioids. The problem is, there is only so much pain a patient can be expected to bear, and so far, only opioids have been available to relieve it.
But that may be about to change. New research into the underlying molecular mechanisms of opioids has made possible the discoveries of new compounds that might just allow for the relief of pain without some of the worst side effects of traditional opioids. (Science writer Bethany Brookshire recently wrote about some of these new compounds for Science News.) If this research bears fruit, morphine may soon go the way of the 19th century bone saw—making way for a revolution of new drugs that don't cause physical dependence, and on which it is impossible to overdose. Drugs for which the risk of addiction will be negligible, or even disappear entirely.
If they pan out.
The Double Door
Traditional opioids—including morphine, the potent synthetic fentanyl and the Vicodin you get from your dentist—all work by binding to opioid receptors in the nervous system. These receptors come in three flavors: mu, delta and kappa. It’s at the mu-opioid receptor that opioids work their magic, activating a cascade of cellular signaling that triggers their pain-relieving effects. In the language of neuroscience, opioids are mu-receptor “agonists,” as opposed to “antagonists,” which are compounds that bind to a receptor and block it, preventing cellular signaling. When an opioid binds with the mu-opioid receptor, it ultimately turns down the volume on the nerves communicating pain. This, of course, is the desired effect.
Unfortunately, that’s not all it does. Opioids also release the neurotransmitter dopamine, which causes euphoria and can lead to addiction. These compounds also inhibit nerve cells from firing more generally, including in parts of the brain that regulate breathing—which can be dangerous. Take too much of an opioid and you stop breathing and die; that’s what it is to overdose. The CDC estimates that 91 Americans die every day from an opioid overdose. The side effects go on, from constipation to nausea to the rapid development of tolerance so that ever higher doses are needed for the same effect.
For a long time, it was thought that this was just the package deal. That to achieve relief from pain, you had to live with the side effects, since they were the result of mu-opioid receptor signaling. Then came Laura Bohn, who set the stage for a new science of pain relief.
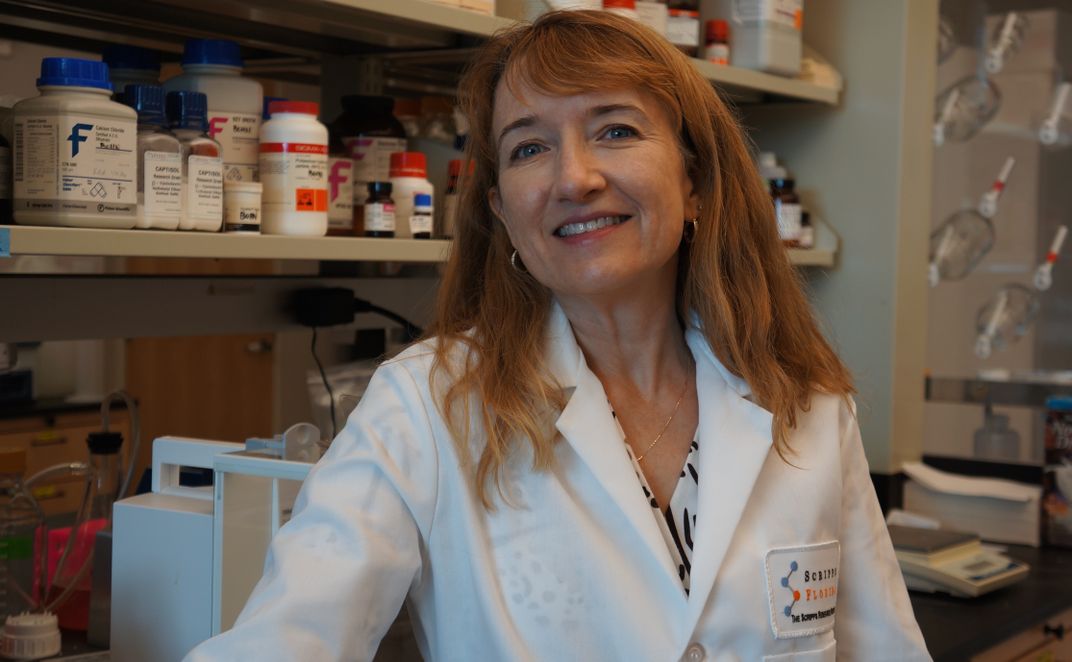
In 1999, Bohn was a post-doctoral researcher in the Marc Caron lab at Duke University studying how the opioid receptor functioned in mice. This was basic research at the time—that is, it wasn’t undertaken as part of a plan to develop new pain drugs. Rather, she says, it was the kind of science for science’s sake that gets eyed for budget cuts. “You remember from the 1980s, all the politicians would say, ‘Putting a mouse on a hot plate, how can this help?’” says Bohn, who is now a pharmacologist at the Scripps Research Institute in Jupiter, Florida. “Well, this is how that helps.”
At the time, researchers knew that there were two proteins involved in opioid receptor signaling: the G-protein, and another called beta-arrestin. To explore the function of beta-arrestin, Bohn took a group of beta-arrestin “knockout” mice—animals who had been genetically manipulated so their bodies contained no beta-arrestin—and gave them morphine alongside a control group of regular mice. It was well known how mice reacted to morphine, so any different response in the knockout mice would provide clues to the role of beta-arrestin.
When you give them morphine, normal mice tend to run around in apparent glee. The knockout mice did not. “When we started treating the animals with morphine, it was just really obvious the difference between the wild types and the ones that lacked the beta-arrestin,” Bohn says. “Obvious to the point where a six-year-old child walked into the lab and said, ‘those mice are different from the other mice.’” Later research showed even more promising signs: The knockout mice showed less constipation and respiratory depression when given morphine, and the morphine proved more potent at relieving pain.
Suddenly, it appeared that the double-edged-sword hypothesis wasn’t necessarily true. The effects of opioids, it seemed, didn’t have to be a package deal—you could spin off some desired effects, and leave others. As Trevena’s Violin puts it: “In the absence of beta-arrestin, morphine was a better drug.”
The key discovery was that opioid “receptors are not on/off switches,” explains Bohn. “It’s not the ‘lock and key,’ where the key goes in and turns the lock and it just opens.” Instead, the receptor is like a double garden gate that can open onto two pathways, the G-protein and beta-arrestin paths. Use morphine to unlock the gate, and it swings open as one unit onto both paths. Change the gate itself so the beta-arrestin side remained locked—as in Bohn’s knockout mice—and you could open to just the G-protein path and reap the crucial benefits of morphine with fewer side effects.
It may not always be the case, Bohn says, that side effects and desired effects will be split neatly into beta-arrestin and G-protein signaling at every receptor. But “these are things we have to learn," she says. "It kind of calls us back to basic research and really understanding the physiology.”
The problem is, you can’t change the mu-receptor gate itself in humans; that would require genetic manipulation before birth. What was needed, therefore, was a different set of keys: New drugs, G-protein “biased-agonists,” which would open only the G-protein side of the gate, and leave the Pandora’s box of harmful side effects safely locked. In 2004, Bohn began looking for those keys; she would be joined in 2008 by the folks at Trevena. “They took this toward a drug development path and I took it toward an academic path,” Bohn says. “I think we are all kind of coming around and seeing that yes, there is some promise to this.”
The New Morphine(s)
In terms of getting onto the market and into patients' prescriptions, Oliceridine is currently leaps and bounds ahead of its competitors. But it isn’t the only drug showing promise. Another compound, known as PZM21, appears to depress respiration—meaning to slow or impede breathing—to a lesser degree than even Oliceridine in rodents, according to work published in the journal Nature in September. There are also indications that it could be less rewarding, i.e., less addictive than traditional opioids.
Like Oliceridine, PZM21 is a biased-agonist opioid compound, but it has a different chemical structure. Scientists are still unclear what about that difference in structure accounts for the different effects of the two compounds, according to pharmacologist Brian Shoichet of the University of California at San Francisco, one of the authors of the Nature study. “Quite apart from clinical use, PZM21, [Oliceridine] and others, are tool molecules that can help us understand the biology of addiction,” he says. “Coupled to the right pharmacology, it could really expand our opportunities for discovering very new molecules conferring very new biological effects.”
Other lines of inquiry go beyond the Bohn's biased-agonist approach. At the University of Maryland School of Pharmacy, researcher Andrew Coop has spent more than a decade working on a synthetic opioid called UMB425, taking precisely the opposite approach from researchers working on biased-agonists like Oliceridine and PZM21. Rather than designing a drug that is more and more selective in order to hit a specific pathway, he asks, “how about how about going the other way and hit a second target that modulates it?” This approach—using one drug to hit multiple receptors—is known as polypharmacology. The result is a drug that, in rodents at least, relieves pain better than morphine with less development of tolerance.
And that's just the tip of the painkiller revolution. Another example of the polypharmacology approach is the work of Stephen Husbands, a medicinal chemist at Bath University. His compound, BU08028, is structurally similar to buprenorphine, a drug used to treat opioid use disorders. It acts at both the mu-opioid receptor and the nociceptin receptor, which is related to the opioid receptors. In monkeys, Husbands showed BU08028 relieves pain without causing dependence, addiction or depression of breathing.
New pain drugs could be only the beginning. Many receptors in the brain—including the dopamine, serotonin and cannabinoid receptors—can also be targeted using the biased-agonist approach, perhaps yielding better antidepressants or other drugs. Trevena is already studying a compound that acts as a biased-agonist at the delta-opioid receptor as a possible migraine headache medication, according to Violin. Previous drugs that targeted the delta-receptor caused seizures, but Trevena’s compound does not (the theory is that the seizures were being caused by beta-arrestin signaling).
Coop, who hopes to test UMB425 in primates and one day in humans, says all that competition is a good thing. “It’s good to have all these different mechanisms moving forward,” he says. “It enhances our chances that one of these will actually be able to make it.”
A Dose of Caution
The potential for these next-generation opioids is great. But in drug development, nothing is guaranteed. Oliceridine could hit some unforeseen problem in clinical trials; UMB425 could prove too addicting or too toxic in humans. A black market chemist could synthesize one of these new compounds and cause a regulatory backlash. (That’s no abstract concern: Last year, the DEA temporarily announced its intention to place the active components of the Kratom plant into the restrictive Schedule I, following reports of people using the plant to treat pain or opioid addiction. That could impede research on mitragynine pseudoindoxyl, another promising new opioid based on compounds found in Kratom.)
Given some dubious industry promises about addiction and pain drugs in the past, Bohn is especially wary of claiming too much, too soon. “I am very conservative on this because I think we have to be very careful not to repeat the problems of the past and oversell an opiate and say it won’t be addictive—as certain companies did,” she says. Her philosophy going forward is to assume all these drugs will have some risk for addiction, and to treat them with caution. At the same time, even if addiction remains a hazard, drugs that eliminate other side effects will still represent a huge step forward.
Yet Bohn’s approach raises a crucial question: Can addiction ever be fully mitigated—or will painkillers always come with the risk of dark consequences? Decoupling the two certainly seems scientifically possible, says Coop, given the current models of biased-agonism and polypharmacology. But addiction is a many-faceted beast, and there could always be new components that are not yet understood. There may be no magic bullet, Coop concedes. “There have been several false dawns with respect to separating the desired from the unwanted effects of opioids," he says, "and the current approaches may again not translate to treating people in the clinic.”
A little excitement is warranted, in other words, but don’t consign morphine to the hall of medical curiosities just yet. “I think we should proceed carefully, but also realize the tremendous opportunity,” Bohn says. “This is a real opportunity in pharmaceutical development.”
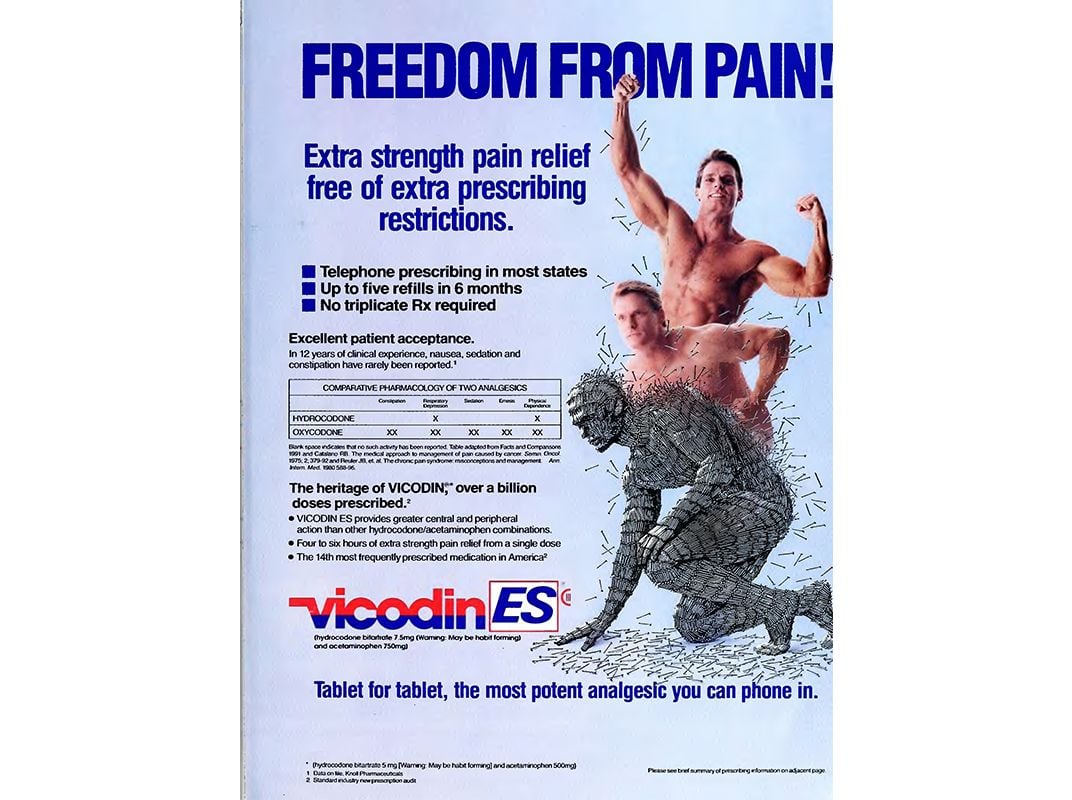
Editor's note, January 16, 2017: Due to an editing error photo caption initially stated that the Vicodin advertisement featured in the North Carolina Medical Journal was published in 1940. Actually, the journal began publication in that year.