F.D.A. Approves New Treatment for Deadliest Strain of Tuberculosis
The drug regimen involves just five pills taken orally for a duration of six months
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/05/be/05be66b8-db03-4ad2-9a9c-1705573183f2/ht_190814_pretomanid_tablet_800x450.jpg)
Seventy-five percent of individuals who contract extensively drug-resistant tuberculosis die before receiving a diagnosis, Donald G. McNeil Jr. reports for the New York Times. Of those who live long enough to seek treatment—an arduous regimen requiring patients to undergo antibiotic injections and take up to 40 pills daily for as long as two years—just 34 percent are ultimately cured.
Still, a new approach developed by the nonprofit TB Alliance is poised to revolutionize treatment for the tens of thousands affected by the so-called XDR strain, as well as the more common multidrug-resistant variation. Instead of subjecting patients to a lengthy cycle of side effect-inducing medications, the BPaL regimen—shown to have a 90 percent success rate when tested on a trial group of 109 participants—cuts the number of drugs down to three: bedaquiline, pretomanid and linezolid. Per Medical Xpress, the treatment involves five pills taken orally for a duration of six months.
Matthew Kavanagh, a health policy expert at Georgetown University, says that pretomanid, newly approved by the U.S. Food and Drug Administration, “could be a major breakthrough.” Speaking with the Los Angeles Times, he adds, “It shifts XDR-TB from most likely a death sentence to likely survivable with effective treatment.”
According to an F.D.A. press release, regulators decided to endorse pretomanid’s use in conjunction with bedaquiline and linezolid, both of which have been previously approved by the agency, due to its “safety and effectiveness,” as demonstrated by the pilot program. The Times’ McNeil explains that the World Health Organization typically follows precedents set by the F.D.A. and its European counterpart, making it likely the treatment will soon be implemented worldwide.
As Linda A. Johnson reports for the Associated Press, the trio of drugs used in the BPaL regimen target tuberculosis in varying ways. They have little known resistance, and though they carry side effects including liver damage, nerve pain and an irregular heartbeat, these issues are far less serious than those associated with antibiotic injections and harsher drug regimens. (McNeil writes that side effects seen with more traditional treatments range from vertigo to deafness, withered nerves, extreme ringing in the ears and even hallucinations; in many cases, these ailments drive patients to abandon treatment regimens completely.)
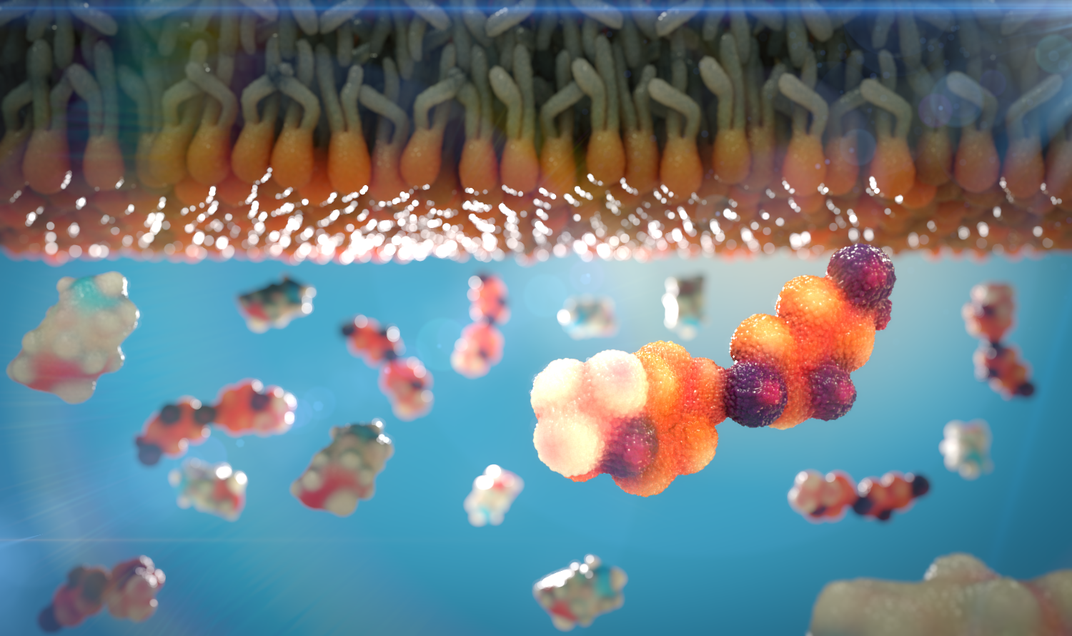
Per the World Health Organization, tuberculosis, an airborne infection most commonly impacting the lungs, affects around 10 million people annually. In 2017, 1.6 million people, including 300,000 H.I.V.-positive patients, died from the disease.
Johnson notes that BPaL proved equally effective for H.I.V.-free trial subjects and those infected with the virus. The drug regimen also appeared to prevent patients from passing along TB within days of starting treatment—a significant deterrence given the ease with which TB bacteria spreads from one person to another.
According to the AP, the pretomanid approach could help more than 75,000 patients per year, particularly in India, China, Indonesia, South Africa and Nigeria. Still, some experts have been wary to embrace the treatment method. As Lindsay McKenna, co-director of the tuberculosis project at the advocacy Treatment Action Group, tells South African newspaper the Daily Maverick, “We are concerned that this regimen, and specifically the new agent pretomanid, was only studied in a small group of 109 patients in the NixTB trial, which goes against the usually stringent requirements of most new medicines.”
Speaking with the Times’ McNeil, Mel Spiegelman, president of the New York-based TB Alliance, argues that a full clinical trial would be impractical, expensive and unethical. South African scientist Francesca Conradie, who was closely involved in the smaller-scale trial, further tells the Daily Maverick that scientists know pretomanid is safe and does not cause heart or liver problems.
“There are many incidences of drugs being registered without a control arm where there were clear benefits to the regimen and where clinicians had no other treatment options,” Conradie says.
Spiegelman also emphasizes the benefits represented by the BPaL regimen, asking McNeil, “Put yourself in a patient’s position. Offered a choice between three drugs with a 90 percent cure rate, and 20 or more with less chance of cure—who would consent to randomization?”
Per the Los Angeles Times, the TB Alliance plans on working with the W.H.O. to efficiently bring pretomanid to the countries where it is needed most.
“For diseases like XDR-TB, where the market in rich countries is small, new models are especially needed,” Georgetown’s Kavanagh says to the Los Angeles Times. Since pretomanid was developed by a nonprofit rather than the pharmaceutical industry, it may be easier for experts to ensure the drug is affordable. Kavanagh concludes, “Many of the recent new drugs for hard-to-treat diseases are not.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/mellon.png)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/mellon.png)