How Epidemics of the Past Changed the Way Americans Lived
Past public health crises inspired innovations in infrastructure, education, fundraising and civic debate
:focal(1987x783:1988x784)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/17/00/1700b1d9-5c50-4f0e-beae-693f1147ff19/children_going_to_a_clinic_for_a_health_check_to_prevent_the_wellcome_l0029944.jpg)
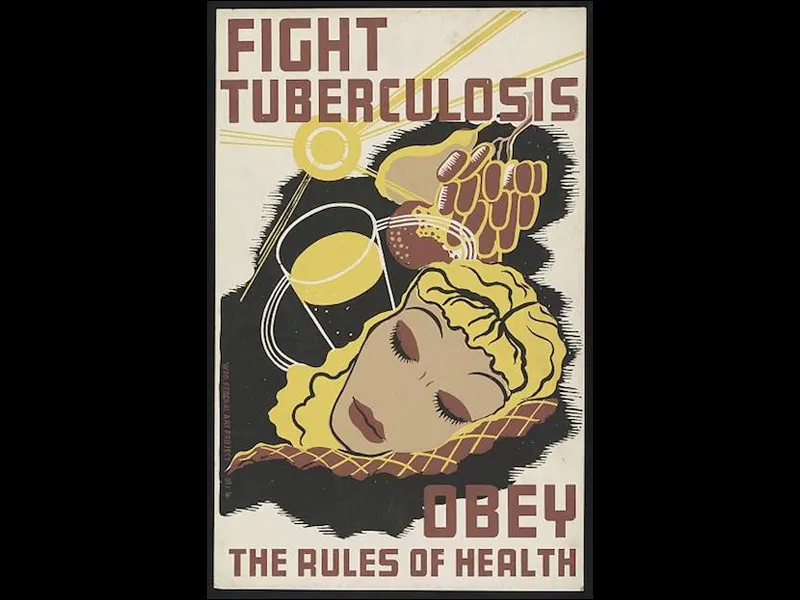
At the end of the 19th century, one in seven people around the world had died of tuberculosis, and the disease ranked as the third leading cause of death in the United States. While physicians had begun to accept German physician Robert Koch’s scientific confirmation that TB was caused by bacteria, this understanding was slow to catch on among the general public, and most people gave little attention to the behaviors that contributed to disease transmission. They didn’t understand that things they did could make them sick. In his book, Pulmonary Tuberculosis: Its Modern Prophylaxis and the Treatment in Special Institutions and at Home, S. Adolphus Knopf, an early TB specialist who practiced medicine in New York, wrote that he had once observed several of his patients sipping from the same glass as other passengers on a train, even as “they coughed and expectorated a good deal.” It was common for family members, or even strangers, to share a drinking cup.
With Knopf’s guidance, in the 1890s the New York City Health Department launched a massive campaign to educate the public and reduce transmission. The “War on Tuberculosis” public health campaign discouraged cup-sharing and prompted states to ban spitting inside public buildings and transit and on sidewalks and other outdoor spaces—instead encouraging the use of special spittoons, to be carefully cleaned on a regular basis. Before long, spitting in public spaces came to be considered uncouth, and swigging from shared bottles was frowned upon as well. These changes in public behavior helped successfully reduce the prevalence of tuberculosis.
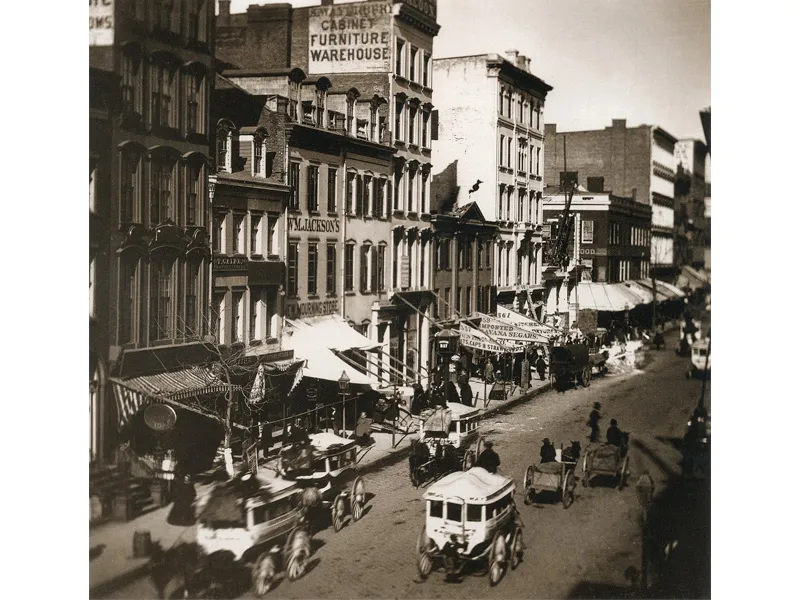
In the 19th century, city streets in the U.S. overflowed with filth. People tossed their discarded newspapers, food scraps, and other trash out their windows onto the streets below. The plentiful horses pulling streetcars and delivery carts contributed to the squalor, as each one dropped over a quart of urine and pounds of manure every day. When a horse died, it became a different kind of hazard. In “Portrait of an Unhealthy City,” Columbia University professor David Rosner writes that since horses are so heavy, when one died in New York City, “its carcass would be left to rot until it had disintegrated enough for someone to pick up the pieces. Children would play with dead horses lying on the streets.” More than 15,000 horse carcasses were collected and removed from New York streets in 1880. Human waste was a problem, too. Many people emptied chamber pots out their windows. Those in tenement housing did not have their own facilities, but had 25 to 30 people sharing a single outhouse. These privies frequently overflowed until workers known as “night soil men” arrived to haul away the dripping barrels of feces, only to dump them into the nearby harbor.
As civic and health leaders began to understand that the frequent outbreaks of tuberculosis, typhoid and cholera that ravaged their cities were connected to the garbage, cities began setting up organized systems for disposing of human urine and feces. Improvements in technology helped the process along. Officials began introducing sand filtration and chlorination systems to clean up municipal water supplies. Indoor toilets were slow to catch on, due to cost, issues with controlling the stench, and the need for a plumbing system. Following Thomas Crapper’s improved model in 1891, water closets became popular, first among the wealthy, and then among the middle-class. Plumbing and sewage systems, paired with tenement house reform, helped remove excrement from the public streets.
Disease radically improved aspects of American culture, too. As physicians came to believe that good ventilation and fresh air could combat illness, builders started adding porches and windows to houses. Real estate investors used the trend to market migration to the West, prompting Eastern physicians to convince consumptives and their families to move thousands of miles from crowded, muggy Eastern cities to the dry air and sunshine in places like Los Angeles and Colorado Springs. The ploy was so influential that in 1872, approximately one-third of Colorado’s population had tuberculosis, having moved to the territory seeking better health.
Some of this sentiment continues today. While we know that sunshine doesn’t kill bacteria, good ventilation and time spent outside does benefit children and adults by promoting physical activity and improving spirits—and access to outdoor spaces and parks still entices homebuyers. This fresh-air “cure” also eventually incited the study of climate as a formal science, as people began to chart temperature, barometric pressure and other weather patterns in hopes of identifying the “ideal” conditions for treating disease.
Epidemics of the past established an ethos of altruism in the U.S. During the 1793 yellow fever epidemic, Philadelphians selflessly stepped up to save their city. With no formal crisis plan, Mayor Matthew Clarkson turned to volunteers collect clothing, food and monetary donations; to pitch a makeshift hospital; and to build a home for 191 children temporarily or permanently orphaned by the epidemic. Members of the Free African Society, an institution run by and for the city’s black population, were particularly altruistic, providing two-thirds of the hospital staff, transporting and burying the dead and performing numerous other medical tasks.
A 20th-century diphtheria outbreak in a small region in the Alaska Territory inspired a national rally of support—and created the Iditarod, the famous dog sled race. When cases of “the children’s disease” began to mount in Nome, Alaska, in January 1925, the town was in trouble. Diphtheria bacteria produces a toxin, making it especially deadly, unless the antitoxin serum is administered. This serum had been readily available for decades, but Nome’s supply had run short, and the town was inaccessible by road or sea in the winter. Leaping into action, 20 of the area’s finest dogsled teams and mushers carried a supply of the serum all the way from Fairbanks—674 miles—in record time, facing temperatures of more than 60 degrees below zero. Their delivery on February 2nd, plus a second shipment a week later, successfully halted the epidemic, saving Nome’s children from suffocation. Newspapers across the country covered the rescue. It was also memorialized in movies (including the animated Balto), with a Central Park statue—and, most notably, with the annual Iditarod race. The significant challenges of delivery by dogsled also sparked investigation into the possibilities of medical transport by airplane, which takes place all the time in remote areas today but was still in its infancy at the time.
Diseases fueled the growth of fundraising strategies. The polio epidemic of 1952 sickened more than 57,000 people across the United States, causing 21,269 cases of paralysis. The situation became so dire that at one point, the Sister Kenny Institute in Minneapolis, a premier polio treatment facility, temporarily ran out of cribs for babies with the disease. In response, the National Foundation of Infantile Paralysis (NFIP), which had been founded in 1938 by President Franklin D. Roosevelt and later came to be known as the March of Dimes, distributed around $25 million through its local chapters. It provided iron lungs, rocking chairs, beds and other equipment to medical facilities, and assigned physicians, nurses, physical therapists, and medical social workers where they were needed. The March of Dimes success has served as the gold standard in public health education and fundraising since its heyday in the 1940s and 1950s.
Public health emergencies have inspired innovations in education. Starting in 1910, Thomas Edison’s lab, which had invented one of the first motion picture devices in the 1890s, partnered with anti-TB activists to produce short films on tuberculosis prevention and transmission—some of the first educational movies. Screened in public places in rural areas, the TB movies were also the first films—of any type—that viewers had ever seen. The anti-tuberculosis crusade was also a model for later NFIP efforts to combat polio that relentlessly put that disease at the front of public agenda until an effective vaccination was developed and implemented, and set a standard for future public health campaigns.
Past epidemics fueled the growth of civic debate and journalism in the U.S., too. As far back as colonial times, newspapers built their audiences by providing an outlet for debate on controversial issues, including disease. Founders of the New England Courant—the first paper in Colonial America to print the voices and perspectives of the colonists—launched their paper as a vehicle to oppose smallpox inoculation during the 1721 Boston epidemic. As smallpox ravaged the city, a Boston doctor named Zabdiel Boylston began using inoculation, a practice in which people are intentionally infected with a disease, to produce milder cases and reduce mortality risk. Backed by those opposed to the practice, James Franklin started the Courant to serve as a tool to fight it. Inoculation’s success was demonstrated in 1721 and later smallpox epidemics, eventually convincing even staunch opponents of its value—but by inspiring an outlet to air their concerns, the anti-inoculation camp had made an important contribution to public discourse.