This Band-Aid-Like Patch Could Detect Early COVID-19 Symptoms
Northwestern University scientist John Rogers has developed a wearable that adheres to the throat and relays data to a physician
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/0d/a7/0da7593d-44a7-4779-90ff-a020c57da882/john_rogers_covid-19_wearable.jpg)
Humans are almost constantly connected to devices and electronics that generate a significant amount of data about who they are and what they do. Many commercially available products like Fitbits, Garmin trackers, Apple watches and other smartwatches are designed to help users take control of their health, and tailor activities to their lifestyle. Even something as unobtrusive to wear as a ring can collect data on sleep patterns, body temperature, heart rate variability, calorie burn, and steps, and even go a step beyond to analyze these biostatistics and package the information so it can be read on a user’s smartphone. Similar, less common but more precise monitoring devices are also being used at clinics and hospitals to help health care providers individualize treatments for a range of conditions from cardiac care to stroke rehabilitation.
Researchers working to contain COVID-19 are increasingly turning to these sleek new wearables for a diagnostic solution. But there is some debate about the best way to do so. Can commercially available devices be leveraged as a tool, or would clinical-grade wearables be more effective?
In April, the Journal of the American Medical Association identified fever, cough and shortness of breath as primary symptoms in both positive and false negative COVID-19 cases. Around the same time, medical thought leaders in the Chicago area approached John Rogers, the director of Northwestern University’s Querrey Simpson Institute for Bioelectronics. Rogers and his team are known for developing next-generation, flexible, wearable devices with clinical-grade monitoring capability that mount on relevant body areas. The patches look and feel much like a Band-Aid, but contain biosensors, onboard memory, data processing and wireless transmission features.
The quality of data the devices can capture is high enough that they can reliably be used in settings and on patients with limited hospital access to run specialty-care tests like electrocardiograms (EKGs). Others reduce the need for complicated machines used to monitor premature infants in intensive care units. For example, the Rogers Research Group works in partnership with the Bill and Melinda Gates Foundation to deploy devices in India, Pakistan and several areas throughout Africa that capture information about maternal and newborn health.
“We were asked whether we could adapt, modify and customize those technologies to COVID-19 patients and specific symptoms associated with that disease,” says Rogers.
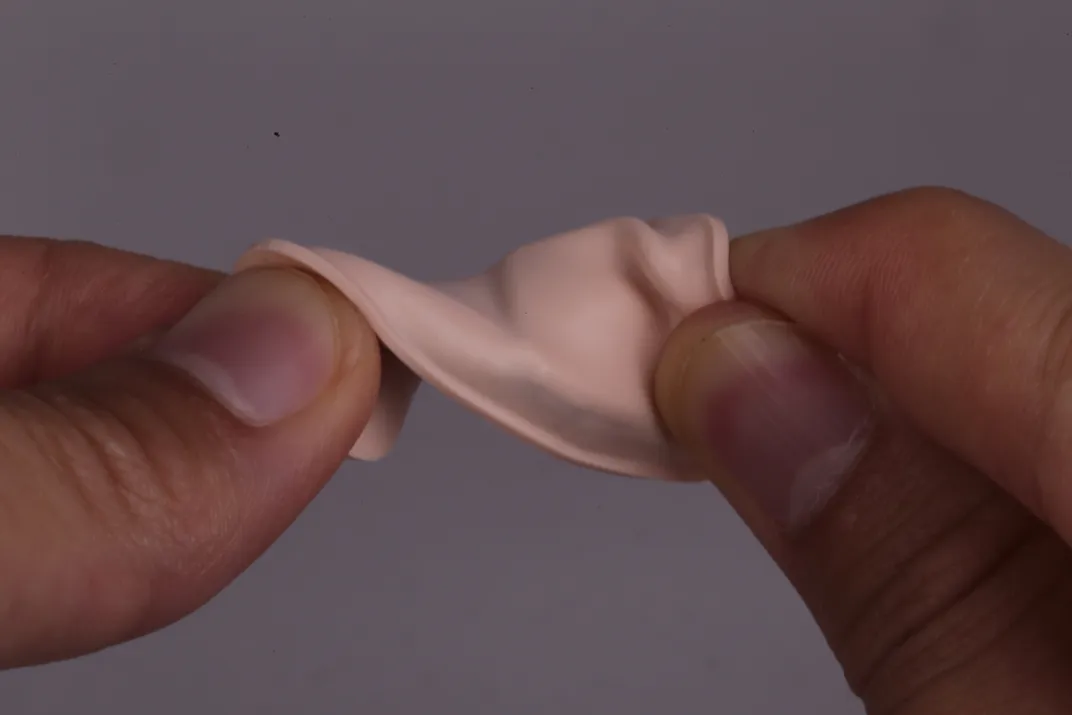
As it turned out, one of the wearable models being used to help rehabilitate stroke patients who had difficulty speaking and swallowing at Chicago’s Shirley Ryan AbilityLab was already well-suited to detecting the respiratory symptoms associated with COVID-19. The soft, flexible rubber patch adheres to an individual’s skin at the dip in the base of the throat. At that location, it can measure tiny vibrations and sense biomarkers like frequency, intensity and sound of coughs and breathing, as well as respiratory rate and effort. Because it is close to the carotid artery, the patch can also pick up blood flow signatures to monitor heart rate.
“As far as monitoring breathing and respiration, you can do that very effectively here,” says Rogers, pointing to his throat, “but you can’t do it right here”—Rogers indicates the wrist, which is where similar commercially available, consumer grade health trackers like FitBits and smartwatches collect data.
The Rogers team added temperature sensors and pulse oximeters—which allow continuous monitoring of low blood oxygen levels, a silent but alarming symptom also associated with COVID-19—to the throat-mounted devices, and deployed them in a pilot study to patients, physicians, nurses and rehabilitation specialists at AbilityLab and at Chicago’s Northwestern Memorial Hospital. For health care providers, especially, early detection of COVID-19 symptoms could have a significant impact on preventing the spread of infection to fellow providers and to non-COVID-19 patients.
“We developed the devices to operate in a completely automated fashion, in the sense that there are no switches or buttons and no software the user has to grapple with,” says Rogers. “The device is recording continuously so there are no gaps in the data, and that turns out to be really important because what we’ve seen with several of these patients is they have very brief transitory periods of spikes in heart rate, for example.”
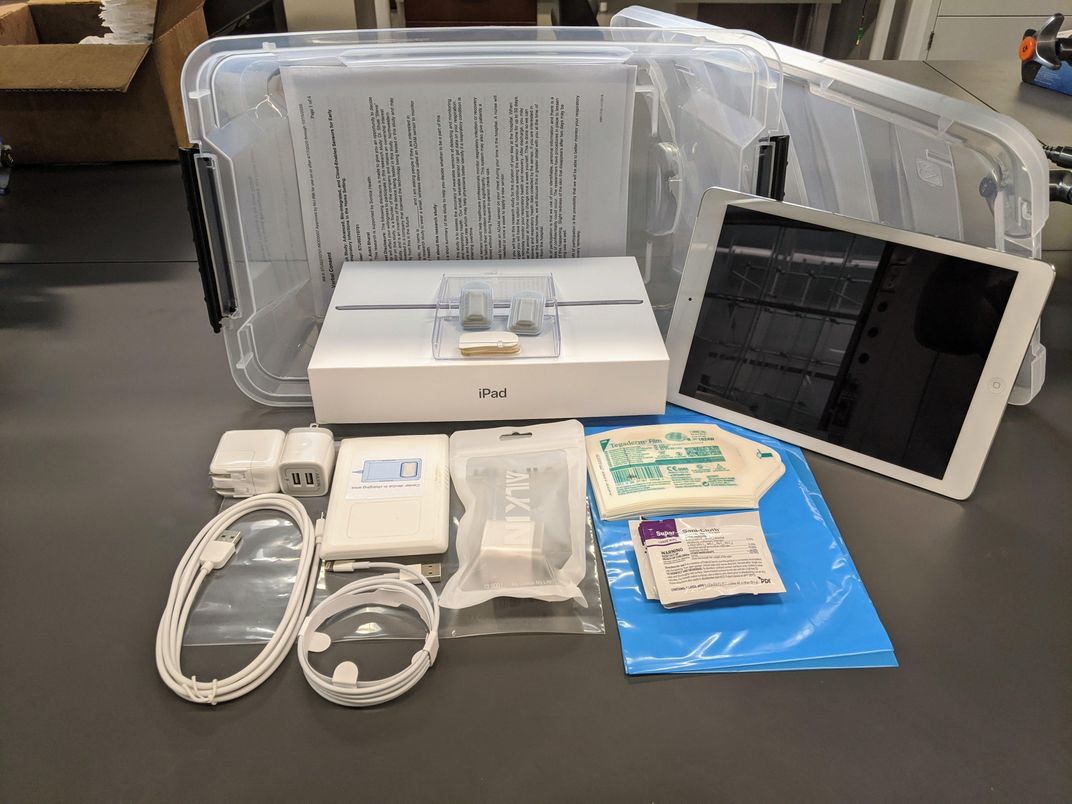
But where does all of the data go, and who is responsible for analyzing it? Biometric values that are recorded on the devices upload to a user’s iPad, then get sent to HIPPA-compliant cloud-based storage and eventually to a dashboard interface where physicians can review daily changes and look for any sign of fever or irregularity in respiration rate for each patient or health care worker under their supervision.
The researchers have collected more than 3,000 hours of data on subjects from the tests, which, in addition to monitoring for illness, are now being used by machine-learning experts and doctors working with healthy control groups to strengthen the device’s algorithms to better detect the nuances of various conditions, including different stages of COVID-19.

Arun Jayaraman, director of the Max Nader Center for Rehabilitation Technologies and Outcomes Research at AbilityLab, says his team has collected data on COVID-19 positive patients, healthy people in the hospital and in the community, as well as patients in the hospital who are ill with other conditions. By comparing all of these various states, “we’re able to predict with pretty high accuracy if a person is having COVID-like symptoms,” says Jayaraman. But different participants show a range of signs and symptoms. So, with all of the comparative data, the researchers are training the algorithm to differentiate between something like an asthma cough versus a COVID-19 cough, which has a distinct signal. So far, however, that device training is still skewed toward those who already have or have had COVID-19.
“What we want to do at the next stage is move on to early symptoms. As people are lining up at testing centers, we want to catch them then, and then create an algorithm which can detect early symptoms, and then use that as a tool which we can use every day in home and in the community,” says Jayaraman. This will depend on additional participants in the community volunteering their data. Jayaraman’s hope is that eventually they can develop a tool that can be readily available at a local pharmacy.
Michael Snyder, director of Stanford University’s Center of Genomics and Personalized Medicine, doesn’t think a clinical-grade device is necessary to achieve this goal. Why not leverage the popularity and price point of wearable devices with health tracking abilities already in the public realm to protect a higher percentage of the general public, he asks. Tens of millions of Fitbits, Apple watches and other smartwatches were sold in 2019, and Snyder, who focuses on precision medicine—creating therapies targeted to individuals’ genetics, lifestyle and environment—thinks these commercially-available devices can be just as effective at early detection as clinical-grade models.
“Our algorithms have to be tuned to the device, but they can be generally device agnostic, and then we can reach tens of millions of people instantly,” he says.
Snyder is currently collecting data on people with COVID-19, or at high risk, through the Stanford Healthcare Innovations Lab in partnership with Fitbit, Garmin and other companies selling wearables. Preliminary results using these devices in COVID-19 patients show that continuous monitoring of heart rate can be especially useful. A chart of one patient’s heart rate, for instance, over the course of several weeks overlaid with their date of symptom onset and diagnosis revealed a sustained increase in heart rate from their normal resting rate nine days before a positive diagnosis.
“On 31 patients we’ve analyzed, we see heart rate spikes three to four days on average, some as many as ten days, before symptoms emerge,” says Snyder.
Because some evidence suggests people can be contagious prior to developing symptoms as well as while infected but asymptomatic, disease spread could be curbed in such individuals who were self-monitoring heart rate and noticed a change that prompted self-quarantine.
Data collection from both clinical and commercial grade devices raises concerns over privacy issues and potential discrimination based on health status. But as the health care industry moves more toward precision medicine and tele-health therapies, especially in the wake of COVID-19, quality of care for individuals suffering any treatable affliction could take precedence for patients, providers, manufacturers and insurances companies, alike.
Oura, a company that manufactures a ring-like wearable is sponsoring similar research at the University of California, San Francisco, by disseminating rings to health care workers and comparing data with their general population users. But, Rogers and his co-authors say these devices are still limited in the specificity and accuracy of data they can gather, and do not as yet offer pulse oximetry or high-fidelity breathing rate measurements. Nor are they approved for remote monitoring by the Food and Drug Administration (FDA).
In response to these issues, Rogers and his colleague Shuai Xu’s tech startup Sonica Health will use their materials along with information from the AbilityLab studies, in partnership with the U.S. Department of Health and Human Services Biomedical Advanced Research Deployment Authority (BARDA) and Sibel Health, to submit a patch device called ADAM with a pulse oximeter and its algorithms to the FDA for approval later this month.
For the duration of the COVID-19 pandemic, collaborators hope that the devices emerging from this research will offer a means for people to engage in public spaces more safely. “It’s not possible to get a nasal swab every day, but this [kind of monitoring] can be done every day by civilians, people coming to work, going to restaurants,” says Jayaraman. “We would like to commercialize it. We would like to offer it to the world. We would like the country to use it.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Sexton_Remy.jpg)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Sexton_Remy.jpg)