Is COVID-19 the Tipping Point for Telemedicine?
Sheltering in place has pushed virtual health care into the mainstream, making us wonder if we’ll ever go back to waiting rooms
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/54/78/5478d7cf-4dc1-45ee-998b-ca095579ec00/telemedicine.jpg)
In February — the month before COVID-19 hit Boston — Partners Healthcare, the huge health system that includes Massachusetts General Hospital, treated 1,600 patients via video visits.
By April, the number of patients seeking care through Partners’ video service had swelled to 242,000.
“We’re not the only ones,” said Joe Kvedar, a dermatology professor at Harvard Medical School and a telemedicine advocate at Partners for three decades, in a May webinar. The same thing was happening across the country as the COVID-19 pandemic made in-person visits at doctors’ offices dangerous for patients and clinicians alike.
Regardless of when the COVID-19 threat dissipates, video visits have crossed a tipping point to become a mainstream way to obtain care, says cardiologist Joe Smith, coauthor of an overview of telemedicine in the Annual Review of Biomedical Engineering. “I don’t think we go back,” he says. “For a long time, hospitals have been the cathedrals of health care where patients have to come. But people are now seeing that they can get their health care in the safety and comfort of their own home.”
Video visits are a form of telemedicine, a term used for technology-enabled ways to deliver virtual medical care (some also use the term telehealth in this context). Telemedicine includes phone calls and secure email, of course, but a lot more as well. Heart-failure patients can be “remote-monitored” in their homes, for example; a smartphone app can alert digestive-disease patients about problems before they occur; and knee-replacement patients can receive physical therapy at home from a virtual assistant named VERA.
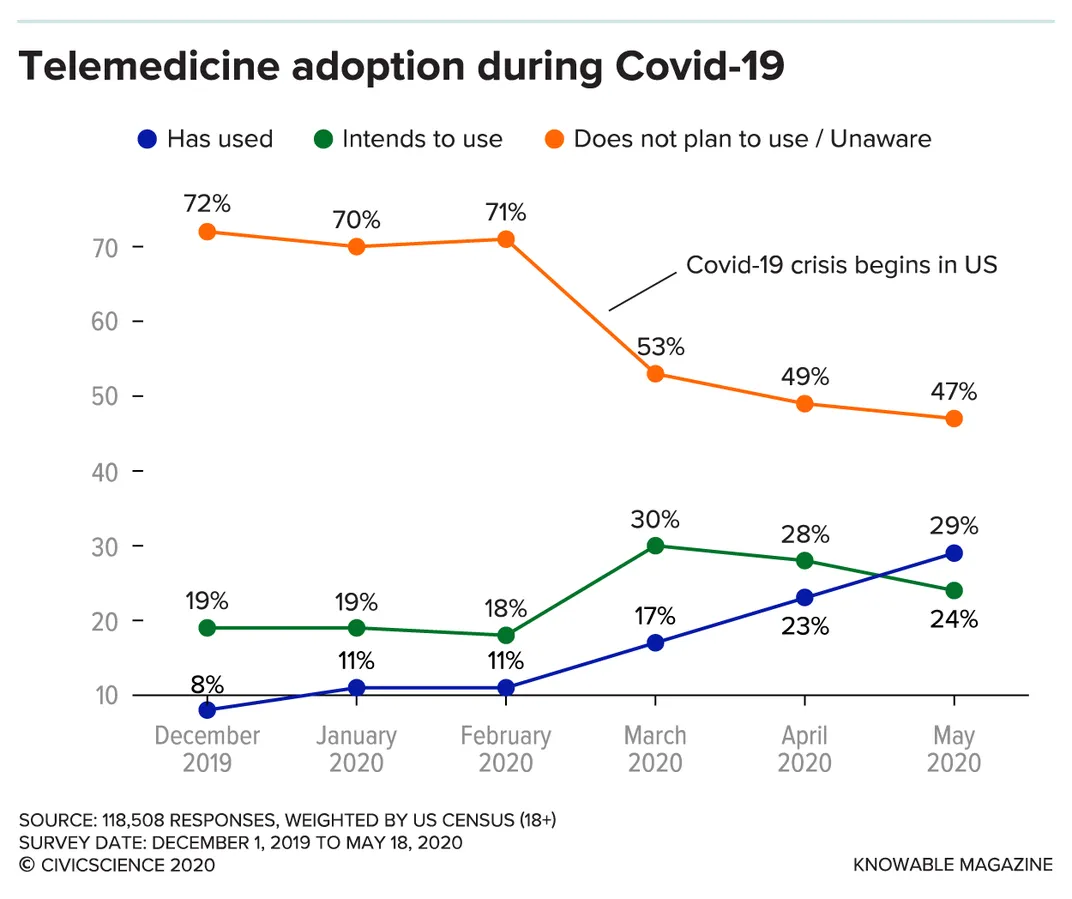
Video visits, primarily offered by commercial companies like Teladoc and AmWell, have become more frequent over the years. But they have never become common. Smith, who now runs two telemedicine companies, says that disincentives such as lower payments than for in-office visits and required changes to office processes have discouraged physicians and health systems from embracing them. Thus, many patients are simply unfamiliar with video-delivered care.
“We adopt technology probably slower than any other industry in the U.S.,” Smith adds. “A rubric inside of health care is that change is bad even if it’s change for the better. So it’s been a real challenge.”
Telemedicine has been bedeviled by myths, wrote Judd Hollander, an emergency physician with Jefferson Health in Philadelphia, in the New England Journal of Medicine Catalyst. It’s “too hard,” “virtual visits are not effective,” “there is not a payment model” and more.
All were swept away this spring when, in a matter of days, the pandemic forced physicians, insurers, regulators and patients to figure out how to make live-video health care work.
That’s one positive thing to come out of COVID-19, says neurologist Michael Okun, national medical director for the Parkinson’s Foundation. “We accomplished in 10 days what we have been trying to do for 10 years — fighting and advocating and trying to get telemedicine up and going,” he says.
Leap forward, step back?
When medical clinics started closing their doors to stymie the spread of COVID-19, physicians went home and regulators went to work. Within weeks, hundreds of federal and state telemedicine rules were changed — in most cases, temporarily — to allow doctors to quickly pivot the way they practiced medicine.
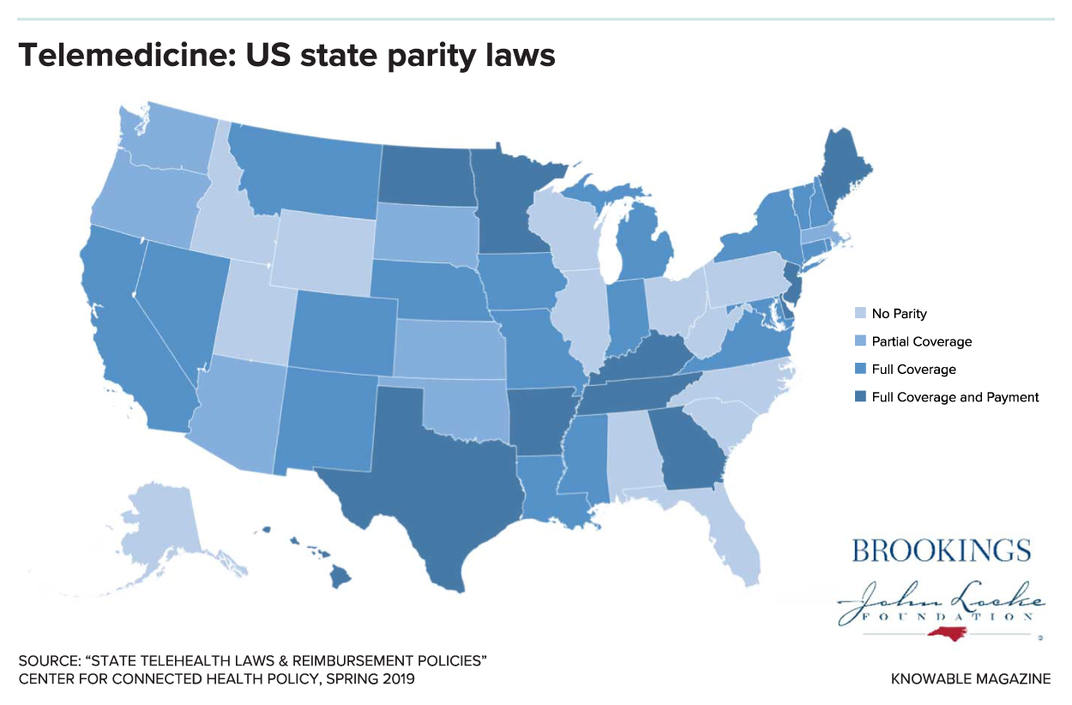
The rules have long been a morass. Telemedicine is regulated at the state level, and no two states are alike. Georgia, for example, requires that private insurers pay the same for telemedicine visits as they do for in-person care, according to the nonprofit Center for Connected Health Policy. But cross the state line to South Carolina and no such “payment parity” exists. For patients insured by Medicaid in New Jersey, video visits are limited to mental-health services. Next door in Delaware, Medicaid will pay physicians, nurse midwives, audiologists and other health-care professionals licensed by the state for care delivered via live video. All states allow video visits for some types of care to Medicaid-insured citizens, but many do not allow care via telephone.
The federal Medicare program, which covers more Americans than any other payer, has its own set of rules. Until now, patients enrolled in Medicare generally could not receive telemedicine services in their homes. In fact, Medicare paid for routine video visits only if a patient lived in a rural area and, even then, the patient had to travel to a local hospital or clinic for a video hook-up with a physician in a different location.
COVID-19 upended everything. All states relaxed their telemedicine rules and, by early March, Medicare was paying for care delivered by telephone, email or video for any diagnostic or treatment purpose in patients’ homes, rural or otherwise. What’s more, Medicare gave a thumbs-up to Skype, FaceTime, Zoom and other platforms. Pre-COVID, those would have been strictly prohibited under the Health Insurance Portability and Accountability Act of 1996, which regulates the privacy and security of health information.
Most of the changes were enacted as temporary measures just to get through the COVID-19 crisis. But Mei Wa Kwong, the Center for Connected Health Policy’s executive director, expects that some of them will become permanent. “I don’t think all of these relaxations will stick around, but I don’t think we will revert back to what we had before COVID-19,” she says.
Medicare’s vast expansion of services that can be delivered by telemedicine is likely to hold, for example. Allowing physicians to examine patients over FaceTime and other non-secure platforms? That will probably go away.
As they consider telemedicine restrictions going forward, regulators are going to be hearing from patients who, until now, have not been vocal telemedicine advocates. “Now that ordinary people are getting a crash course in telehealth, that this how you can receive health-care services, they will be become an important voice post-COVID-19 that will make it a little harder for policymakers to ignore,” Kwong says.
How good is video care?
Can video visits be trusted to offer the same quality of care as traditional in-person visits when those become safe again? “That’s a horrible question,” Hollander says.
Telemedicine, in his view, offers additional ways — not better or worse ways — to receive care from your doctor. You might, for example, see your cardiologist in person in January, check in via video in February, exchange text messages in March and return to the clinic for a face-to-face in April. If bad weather makes travel difficult in April, jumping on a video visit is better than missing care entirely even if an in-person visit would have been preferred that month.
Nonetheless, as telemedicine goes mainstream, the question of quality deserves attention. There are few published studies so far, and they give conflicting signals. A 2016 review of insurance claims, for example, compared care delivered by Teladoc, a popular direct-to-consumer care company, with that delivered at physicians’ offices. Teladoc performed worse on two measures — appropriate ordering of strep tests and antibiotics for bronchitis — than physicians’ offices, and about the same for appropriate ordering of images for back pain.
And a 2016 report tells how researchers at the University of California, San Francisco, had actors and medical students pose as patients with common conditions — sore throats, urinary tract infections and so forth — and seek care from one of eight companies via telephone, webchat or video. Overall, just 77 percent of the “patients” received a correct diagnosis, and providers followed care guidelines in only 54 percent of the visits. Researchers noted that some video-visit providers did better than others, and they also pointed out that adherence to guidelines and the quality of care also vary widely in face-to-face visits. “If you’re a bad doctor in person, you’re probably a bad doctor via telemedicine,” Hollander says.

In another study, Hollander and three colleagues at Thomas Jefferson University compared the care delivered by Jefferson Health emergency physicians in the emergency department, in an urgent care clinic and via a video visit. The rate of appropriate antibiotic prescribing was at least as good in video-visit care as in the other two settings.
For patients who have trouble traveling to medical appointments, the quality of care is just one factor worth considering. A 2017 randomized controlled trial found that patients with Parkinson’s disease, a degenerative neurologic condition, who had “virtual house calls” with a neurologist had clinical outcomes — such as the number of emergency room visits and number of hospitalizations over 12 months — comparable to those who had regular outpatient visits. But patients who were seen via video in their own homes reported that they felt better than those who received care at a clinic; and each video visit, on average, saved a patient from traveling 38 miles.
Another study showed that care via telemedicine care can save a lot of money. Reflexion Health — Smith is its CEO — provides virtual physical therapy, using an avatar coach and imaging that gives patients real-time feedback on whether they are doing exercises correctly. In a randomized controlled trial published this year, virtual therapy was found to be as effective as traditional in-person therapy for patients rehabilitating after total knee replacement surgery. On average, the avatar-led therapy cost $2,745 less per patient over three months.
Kvedar, who is the current president of the American Telemedicine Association, wants federal and state regulators to adopt permanent policies that make it easy — and financially viable — for health systems to offer video visits. Before COVID-19, his own system’s video-visit program was limited to a virtual urgent-care service where patients could get simple problems — skin rash, sinusitis, urinary tract infection symptoms — checked out. The average wait time for patients was six to seven minutes; in about 80 percent of the cases, clinicians could address the problems via video; and patient-satisfaction scores were high.
When we reach that wonderful nirvana of access, quality and convenience, everyone knows it,” Kvedar says. “And nobody wants to go back.”
