This Implant Could One Day Control Your Sleep and Wake Cycles
The so-called ‘living pharmacy’ will be able to manufacture pharmaceuticals from inside the body
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/29/dd/29dd0dec-ebdf-4ac1-82b3-9856560a2229/jet_lag-main.jpg)
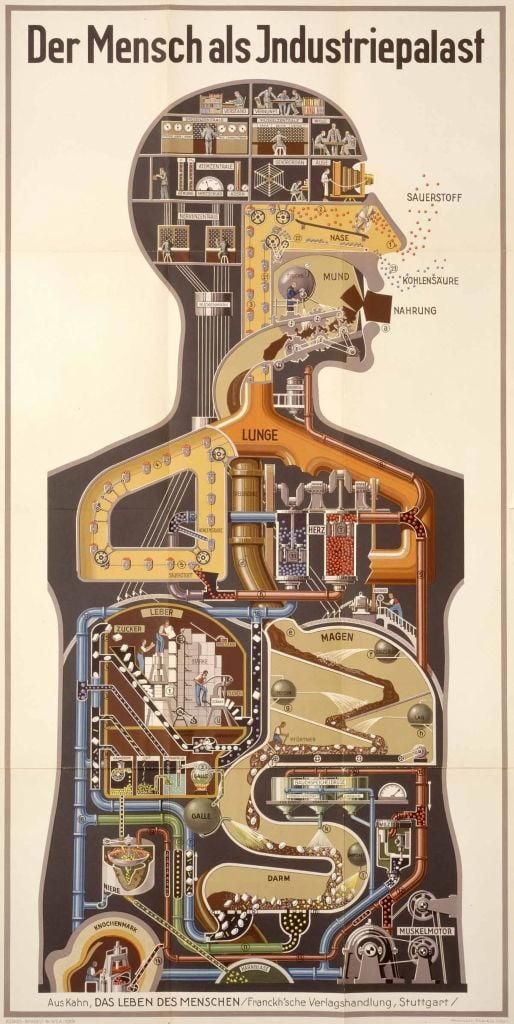
In 1926, Fritz Kahn completed Man as Industrial Palace, the preeminent lithograph in his five-volume publication The Life of Man. The illustration shows a human body bustling with tiny factory workers. They cheerily operate a brain filled with switchboards, circuits and manometers. Below their feet, an ingenious network of pipes, chutes and conveyer belts make up the blood circulatory system. The image epitomizes a central motif in Kahn’s oeuvre: the parallel between human physiology and manufacturing, or the human body as a marvel of engineering.
An apparatus currently in the embryonic stage of development—the so-called “implantable living pharmacy”—could have easily originated in Kahn’s fervid imagination. The concept is being developed by the Defense Advanced Research Projects Agency (DARPA) in conjunction with several universities, notably Northwestern and Rice. Researchers envision a miniaturized factory, tucked inside a microchip, that will manufacture pharmaceuticals from inside the body. The drugs will then be delivered to precise targets at the command of a mobile application. DARPA’s initial, modest goal for the four-and-a-half-year program, which awarded contracts to researchers this May, is to alleviate jet lag.
Jet lag is a disorder of the circadian rhythm—the daily biological rhythm that governs the internal timing of all organisms on Earth. When we fly across time zones, the internal misalignment can cause fatigue, grogginess and disorientation. More than an annoyance for the armed forces, the disorder is considered a threat to the readiness of troops who, upon arriving at far-flung locations, may be called upon to operate at peak performance. Similarly, a 2019 study found that the alertness and job performance of health care workers were severely impaired when working evening shifts. Shift workers of all varieties frequently suffer from circadian rhythm disorders, putting them at greater risk of metabolic syndrome and cardiovascular diseases.
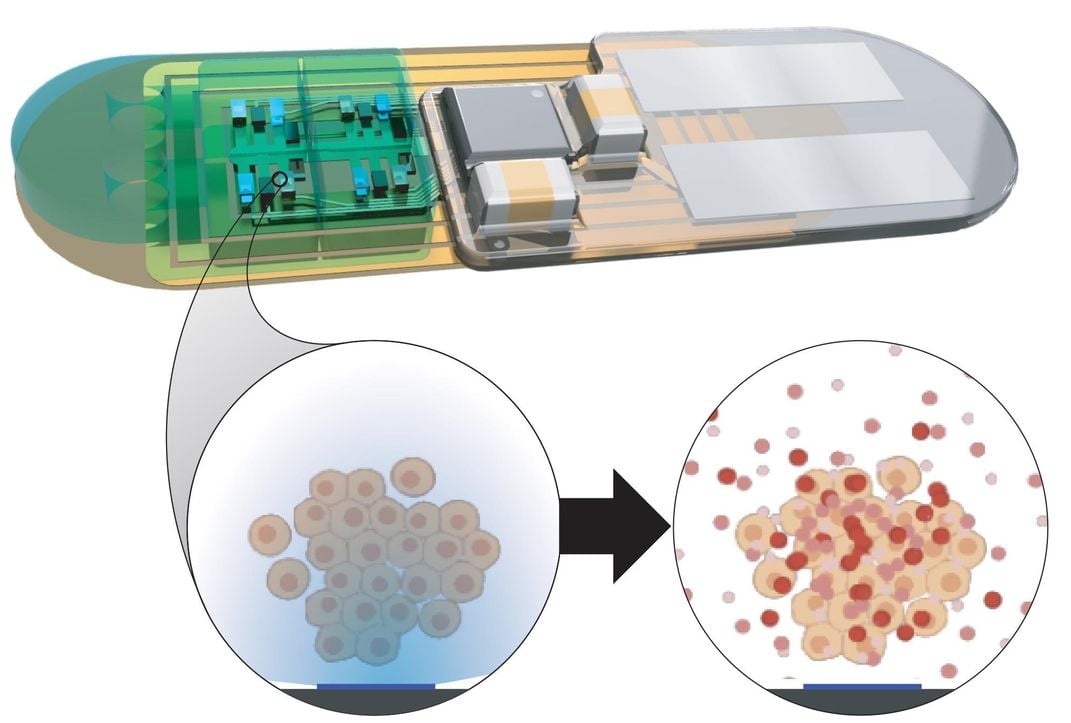
The implantable living pharmacy, which is still in the “proof of concept” stage of development, is actually envisioned as two separate devices—a microchip implant and an armband. The implant will contain a layer of living synthetic cells, along with a sensor that measures temperature, a short-range wireless transmitter and a photo detector. The cells are sourced from a human donor and reengineered to perform specific functions. They’ll be mass produced in the lab, and slathered onto a layer of tiny LED lights.
The microchip will be set with a unique identification number and encryption key, then implanted under the skin in an outpatient procedure. The chip will be controlled by a battery-powered hub attached to an armband. That hub will receive signals transmitted from a mobile app.
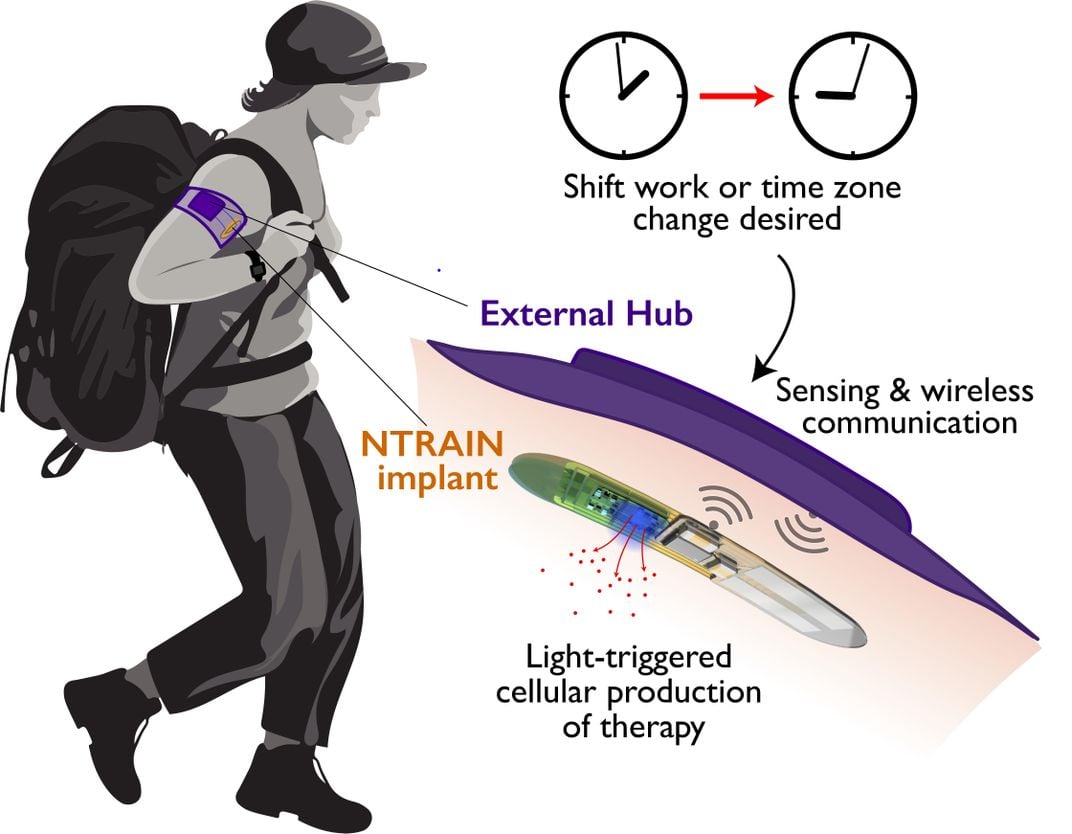
If a soldier wishes to reset their internal clock, they’ll simply grab their phone, log onto the app and enter their upcoming itinerary—say, a flight departing at 5:30 a.m. from Arlington, Virginia, and arriving 16 hours later at Fort Buckner in Okinawa, Japan. Using short-range wireless communications, the hub will receive the signal and activate the LED lights inside the chip. The lights will shine on the synthetic cells, stimulating them to generate two compounds that are naturally produced in the body. The compounds will be released directly into the bloodstream, heading towards targeted locations, such as a tiny, centrally-located structure in the brain called the suprachiasmatic nucleus (SCN) that serves as master pacemaker of the circadian rhythm. Whatever the target location, the flow of biomolecules will alter the natural clock. When the solider arrives in Okinawa, their body will be perfectly in tune with local time.
The synthetic cells will be kept isolated from the host’s immune system by a membrane constructed of novel biomaterials, allowing only nutrients and oxygen in and only the compounds out. Should anything go wrong, they would swallow a pill that would kill the cells inside the chip only, leaving the rest of their body unaffected.
Computer engineer Josiah Hester’s previous project, a Game Boy that can run forever without a battery, was popular and uncontroversial. Now, the Northwestern University professor is coordinating the design of the living pharmacy’s external hub from his Evanston, Illinois lab. Suddenly faced with anxious questions, he patiently describes the safety measures that will be put into place.
To protect against hacking and malware, the user will have to confirm any command they tap into their phone on the hub. User data will be stored in the hub itself; any future moves to the cloud are not being considered at this time. “If a company like Microsoft or Apple were to ever try to integrate this into their products, there would have to be a significant societal discussion about that—this is very sensitive data,” says Hester. The messages traveling from the hub to the app will be encrypted. The armband itself might contain a “kill switch” button that will shut it off immediately. Most importantly, the implant is useless without the armband. At any time, for any reason, the user can simply remove the armband and the microchip will be immediately disabled.
When Jonathan Rivnay, the principal investigator of the project, contemplates the future of biotechnology, his biggest concern is the public perception of his work. The Northwestern University professor of bioengineering describes Luigi Galvani, the 18th century Italian who served as inspiration for Frankenstein. The biologist made his name by tying up headless frogs in his Bologna laboratory and shocking them with jolts of electricity. “He would shock the frog’s leg and then it would kick,” Rivnay explains, grinning broadly. It may have startled society at the time, but the founder of bioelectricity wasn’t quite reanimating the dead. Rivnay is concerned about the public’s tendency to conflate science fiction with scientific research. “There’s a lot of great advances that are happening and they’re not very well communicated to the public,” he says. “People jump immediately to what they’ve seen in a movie and make false connections.” In encouraging signs for the project, some are more than ready to embrace the future. As soon as it was announced, Rivnay began receiving emails from people with severe sleep disorders, offering to sign up to be test subjects.
Russell Foster is head of the Sleep and Circadian Neuroscience Institute at Oxford University. The professor isn’t affiliated with the project, but he’s an enthusiastic proponent of it. He highlights the microchip’s ability to release medication at precise times as a critical benefit, especially for vulnerable populations. “If I had to go into a nursing home and needed to make sure I was getting my medication at the right time, I’d certainly get a microchip,” he says.
If all goes according to plan, remote controllable bio-hybrid microchips could one day become the most intimate form of smart technology in our lives—internal sensors that manage our health as we go about our daily routine, judging via algorithm which drug to make and when to dispense it.
What if, in the near future, children with type-1 diabetes didn’t have to inject themselves with insulin multiple times a day? What if everything could be managed via smart phone? The first voyagers to Mars face a lengthy trip. If the implant comes to full fruition, no need to carry medicine. The drugstore would always be open, inside their bodies, available to produce the pharmaceuticals needed.
The microchip could even potentially be used to augment human performance. What if an Olympic runner could program their cells to produce a burst of adrenaline at the start of a race?
“A user- friendly device that allows the timed delivery of drugs is immensely important,” Foster says. “The concept is brilliant. I applaud their ambition.”
But in the midst of all the excitement, uncomfortable questions beg to be asked.
In Book III of Ovid’s Metamorphoses, young Cadmus, mythological founder of Thebes, stumbles across a dragon. He fights and kills the beast, not knowing it’s sacred, and buries its teeth in a nearby field. When the field is reaped, a crop of fierce warriors spring up from where the teeth had been sown, setting off a chain of tragic circumstances—anguish, bloodshed and ultimately madness—far worse than his original predicament.
As unpleasant as jet lag can be, how does one weigh the consequences of implanting data-storing, signal-transmitting, drug-manufacturing microchips into the bodies of perfectly healthy soldiers? If and when the technology becomes available to the general public, which medical conditions would qualify? Are there healthy people who find popping a pill so arduous and time consuming that they would get microchipped just to avoid the task?
It has all the makings of the latest episode of Black Mirror. Paul Sheehan, the program manager overseeing the development of the chip, is not a fan of the sci-fi anthology series on Netflix. “I could never get past the first episode,” says Sheehan, a chemical physicist who spoke from DARPA’S Biological Technologies Office.
Sheehan explains that the chip will be subject to several rounds of testing before FDA approval. He points to implants currently on the market, like pacemakers and morphine pumps. But he prefers not to speculate on any possible future uses of the device. “For any technology, it’s hard to see where it goes. We’re trying to focus on immediate issues,” he says.
The underlying theme of The Bleeding Edge, the 2018 documentary about the medical device industry, was that “innovative” doesn’t necessarily mean better care. Another 2018 film, Upgrade, warned audiences about “helpful” scientists offering state-of-the-art biotech devices.
While acknowledging safety concerns, Hester is thrilled about working on a microchip that’s so revolutionary. (Implants generally don’t perform many functions.) “RFID chips are lame. They don’t do anything,” he says. “This implant will respond to things happening in the body and adapt in real time.” The team is currently in the design phase. Soon, they hope to begin testing the separate components of the pharmacy on rodent models, eventually getting to a working prototype.
Ultimately, whatever Ovid might say on the subject, the scientists behind the implantable living pharmacy are plowing full steam ahead. They’re designing an impressive marvel of modern engineering. Both smart device and synergistic platform, the microchip integrates the latest innovations in bioelectronics, synthetic biology and computer engineering.
Bioengineer Omid Veiseh is delighted to be working on the project. His lab is part of Texas Medical Center, the largest medical complex in the world. Sometimes, he leaves his office and crosses the street to grab lunch with the clinicians. Whenever he visits, he asks probing questions about their patient’s lives.
Veiseh explains that, if it were left to him working in a vacuum, he might just make cool gadgets. When he visits the hospital, he gains insight into real people’s problems. “There’s a tremendous opportunity to hack into the body, in a good way, and come up with the therapies of the future,” he says. “If we can make this work, it opens up so many possibilities.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Dieynaba_Y.jpg)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Dieynaba_Y.jpg)