What Scientists Know About Immunity to the Novel Coronavirus
Though COVID-19 likely makes recovered patients immune, experts aren’t sure how long protection lasts
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/e1/40/e1406e36-48fe-4f32-b5de-f635a661af13/gettyimages-1212213050.jpg)
Resolving the COVID-19 pandemic quickly hinges on a crucial factor: how well a person’s immune system remembers SARS-CoV-2, the virus behind the disease, after an infection has resolved and the patient is back in good health.
This phenomenon, called immune memory, helps our bodies avoid reinfection by a bug we’ve had before and influences the potency of life-saving treatments and vaccines. By starving pathogens of hosts to infect, immune individuals cut off the chain of transmission, bolstering the health of the entire population.
Scientists don’t yet have definitive answers about SARS-CoV-2 immunity. For now, people who have had the disease appear unlikely to get it again, at least within the bounds of the current outbreak. Small, early studies in animals suggest immune molecules may stick around for weeks (at least) after an initial exposure. Because researchers have only known about the virus for a few months, however, they can’t yet confidently forecast how long immune defenses against SARS-CoV-2 will last.
“We are so early in this disease right now,” says C. Brandon Ogbunu, a computational epidemiologist at Brown University. “In many respects, we have no idea, and we won’t until we get a longitudinal look.”
A memorable infection
When a pathogen breaches the body’s barriers, the immune system will churn out a variety of immune molecules to fight it off. One subset of these molecules, called antibodies, recognizes specific features of the bug in question and mounts repeated attacks until the invader is purged from the body. (Antibodies can also be a way for clinicians to tell if a patient has been recently infected with a given pathogen, even when the microbe itself can no longer be detected.)
Though the army of antibodies dwindles after a disease has resolved, the immune system can whip up a new batch if it sees the same pathogen again, often quashing the new infection before it has the opportunity to cause severe symptoms. Vaccines safely simulate this process by exposing the body to a harmless version or piece of a germ, teaching the immune system to identify the invader without the need to endure a potentially grueling disease.
From the immune system’s perspective, some pathogens are unforgettable. One brush with the viruses that cause chickenpox or polio, for instance, is usually enough to protect a person for life. Other microbes, however, leave less of an impression, and researchers still aren’t entirely sure why. This applies to the four coronaviruses known to cause a subset of common cold cases, says Rachel Graham, an epidemiologist and coronavirus expert at the University of North Carolina at Chapel Hill. Immunity against these viruses seems to wane in a matter of months or a couple of years, which is why people get colds so frequently.
Because SARS-CoV-2 was only discovered recently, scientists don’t yet know how the human immune system will treat this new virus. Reports have surfaced in recent weeks of people who have tested positive for the virus after apparently recovering from COVID-19, fueling some suspicion that their first exposure wasn’t enough to protect them from a second bout of disease. Most experts don’t think these test results represent reinfections. Rather, the virus may have never left the patients’ bodies, temporarily dipping below detectable levels and allowing symptoms to abate before surging upward again. Tests are also imperfect, and can incorrectly indicate the virus’ presence or absence at different points.
Because the COVID-19 outbreak is still underway, “if you’ve already had this strain and you’re re-exposed, you would likely be protected,” says Taia Wang, an immunologist and virologist at Stanford University and the Chan Zuckerberg Biohub. Even antibodies against the most forgettable coronaviruses tend to stick around for at least that long.
COVID-19 packs a stronger punch than the common cold, so antibodies capable of fending off this new coronavirus may have a shot at lingering longer. Broadly speaking, the more severe the disease, the more resources the body will dedicate to memorizing that pathogen’s features, and the stronger and longer lasting the immune response will be, says Allison Roder, a virologist at New York University. Previous studies have shown that people who survived SARS, another coronavirus disease that resulted in a 2003 epidemic, still have antibodies against the pathogen in their blood years after recovery. But this trend is not a sure thing, and scientists don’t know yet whether SARS-CoV-2 will fall in line.
Earlier this month, a team of researchers posted a study (which has yet to be published in a peer-reviewed journal) describing two rhesus macaques that could not be reinfected with SARS-CoV-2 several weeks after recovering from mild bouts of COVID-19. The authors chalked the protection up to the antibodies they found in the monkeys’ bodies, apparently produced in response to the virus—a result that appears to echo the detection of comparable molecules in human COVID-19 patients.
But the mere presence of antibodies doesn’t guarantee protection, Wang says. Reinfections with common cold coronaviruses can still happen in patients who carry antibodies against them. And a bevy of other factors, including a person’s age and genetics, can drastically alter the course of an immune response.
An evolving virus?
Complicating matters further is the biology of SARS-CoV-2 itself. Viruses aren’t technically alive: While they contain genetic instructions to make more of themselves, they lack the molecular tools to execute the steps, and must hijack living cells to complete the replication process for them.
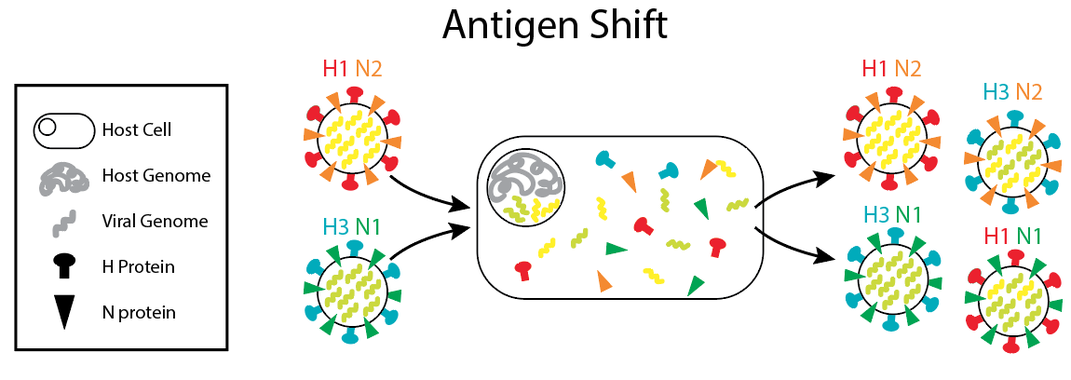
After these pathogens infect cells, their genomes often duplicate sloppily, leading to frequent mutations that persist in the new copies. Most of these changes are inconsequential, or evolutionary dead ends. Occasionally, however, mutations will alter a viral strain so substantially that the immune system can no longer recognize it, sparking an outbreak—even in populations that have seen a previous version of the virus before. Viruses in the influenza family are the poster children for these drastic transformations, which is part of why scientists create a new flu vaccine every year.
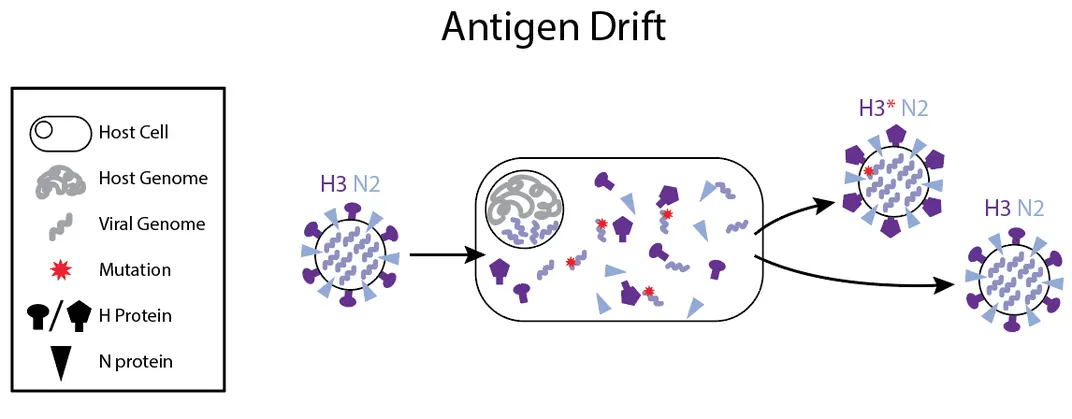
Some viruses have another immunity-thwarting trick as well: If a person is infected with two different strains of the flu at the same time, those viruses can swap genetic material with each other, generating a new hybrid strain that doesn’t look like either of its precursors, allowing it to skirt the body’s defenses.
Researchers don’t yet know how quickly similar changes could occur in SARS-CoV-2. Unlike flu viruses, coronaviruses can proofread their genomes as they copy them, correcting mistakes along the way. That feature reduces their mutation rate, and might make them “less of a moving target” for the immune system, says Scott Kenney, an animal coronavirus expert at Ohio State University. But coronaviruses still frequently trade segments of their genetic code with each other, leaving the potential for immune evasion wide open.
So far, SARS-CoV-2 also doesn’t appear to be undergoing any extreme mutations as it sweeps across the globe. That may be because it’s already hit on such a successful strategy, and doesn’t yet need to change its tactic. “Right now, it’s seeing a completely naive population” that’s never been exposed to the virus before, Graham says. The virus “doesn’t seem to be responding to any kind of pressure,” she adds.
Should SARS-CoV-2 get a second infectious wind, it may not come for some time. Even fast-mutating influenza strains can take years to reenter populations. And if or when that day comes, future COVID-19 outbreaks could be milder. Sometimes viral success means treading gently with the host, says Catherine Freije, a virologist at Harvard University.
“Viruses that causes severe disease actually tend to die out faster because a host that’s feeling ill can’t spread it as well.” In those cases, she says, sometimes, “the outbreak just sort of fizzles out.”
But we can’t rule out the possibility that SARS-CoV-2 could change in a way that bumps up its virulence instead, Kenney says. To steel the population for what’s ahead, sometimes, he adds, “We just have to be the ultimate pessimist when it comes to this type of outbreak.”
Protection without disease
Although much about COVID-19 remains unknown, researchers are racing through vaccine development to boost the world’s collective immunity—something that would stem the spread of the virus through the human population.
“Vaccine development is going to be critical to controlling this outbreak,” says Wang. That’s especially true if SARS-CoV-2 returns for an encore act. “If it’s an ever-present pathogen, we’ll certainly need vaccines to be part of our arsenal.”
Researchers have managed to concoct partially effective vaccines to combat other coronavirus infections in animals, such as pigs. In these creatures, immunity lasts “at least several months, possibly longer,” says Qiuhong Wang, a coronavirus expert at Ohio State University. (Because many of the subjects are livestock, they often don’t live long enough for researchers to test them further.) These vaccines may be reason for hope, she says, pointing out that “humans are animals, too.”
Several research teams are designing human vaccines that trigger the production of antibodies that attack SARS-CoV-2’s spike protein—the molecular key the virus uses to unlock and enter human cells. Because the spike protein is crucial for viral infection, it makes an excellent target for a vaccine, says Benhur Lee, a virologist at the Icahn School of Medicine at Mount Sinai. But Lee also points out that the spike protein, like other parts of the virus, is capable of mutating—something that could compromise the ability of a vaccinated individual to ward off the virus.
If mutation regularly occurs to that extent, scientists may need to frequently reformulate COVID-19 vaccines, like they do with pathogens in the flu family, Wang says. “We’d be starting over to some degree if there is a new outbreak.”
However, Wang cautions that it’s too soon to tell whether that will be the case. As research worldwide proceeds at breakneck speed, scientists may instead be able to brew up a universal vaccine that’s active against multiple forms of SARS-CoV-2.
But vaccines, which require rigorous testing and retesting to ensure efficacy and safety, take a long time to develop—typically more than a year, Qiuhong Wang says. In the meantime, researchers are turning their attention to treatments that could save those who have already been infected.
Some solutions will inevitably require antiviral drugs that tackle active SARS-CoV-2 infections after they’ve already begun, usually by interfering with the virus’ infection cycle.
But another approach, based on a time-tested technique, also taps into the immune response: transferring blood plasma—and the disease-repelling antibodies it contains—from recovered patients into infected ones. Though new to the current pandemic, the treatment has been deployed in various forms since the 1890s, and saw modest success during outbreaks of SARS in 2003 and Ebola in 2014. Ongoing trials in New York are now recruiting carefully screened, healthy volunteers who no longer have symptoms or detectable virus in their bodies to donate plasma. Importantly, this doesn’t diminish donors’ own resistance to SARS-CoV-2, since their immune systems have already learned to manufacture more antibodies.
Antibodies degrade over time, and won’t protect the people who receive these transfusions forever. The plasma treatments also can’t teach their recipients’ immune systems to make new antibodies after the first batch disappears. But this stopgap measure could ease the burden on health care workers and buy time for some of the outbreak’s most vulnerable victims.
Even as the pandemic evolves, researchers are already looking ahead. Just as the response to this outbreak was informed by its predecessors, so too will COVID-19 teach us about what’s to come, Qiuhong Wang says. The entry of other coronavirus strains into our species “is inevitable.”
“We don’t know when or where that will happen,” she says. But hopefully by the time the next pandemic comes around, the world will be more ready.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/10172852_10152012979290896_320129237_n.jpg)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/10172852_10152012979290896_320129237_n.jpg)