Years ago, the scientist Letizia Marsili was skiing with her sister in Trentino, high in the Italian Alps, when she lost her balance on a double black diamond run and crashed shoulder first into the snow. Marsili felt a jolt of pain. Then the pain subsided, so she brushed herself off and headed back to the lifts. By the end of the day, she’d skied another 18 miles.
“Everything was normal,” Marsili told me recently, through an interpreter. “We got back to the lodge, we went to the sauna. I was in such a happy mood.” But over dinner, Marsili noticed that she was having trouble holding her fork and knife—they kept dropping out of her hand. The next day, she got an X-ray. “And the doctor, he said, ‘Well, yes, your shoulder is broken,’” Marsili remembers.
She was shaken, but not surprised. Things like this had been happening as far back as she could remember. Shortly after her sixth birthday, while climbing a pole in a neighbor’s yard in the Tuscan city of Siena, she stuck herself in the side on an errant nail; after stanching the flow of blood, while her friends watched in horror, she pronounced herself fine to keep playing. Later, she twisted her ankle while rock climbing, and kept going; she burned her hands with hot oil. In each situation, the experience was the same: She felt a shudder of discomfort that melted away in seconds.
“I just thought of it as part of who I was,” Marsili told me proudly. “I was strong, I was resilient. I bounced back.” And it wasn’t as if she’d known any different: Her mother, Maria Domenica, and her sister, Maria Elena, had been the same way—masses of scar tissue and healed fractures and bruised shins, juggernauting their way through life.

At the University of Siena, where Marsili has worked since 1998 as a professor of marine ecology, her colleagues took to calling her “Superwoman.” She seemed made of steel, impervious to injury. On summer expeditions to the Sea of Cortez, in the Pacific Ocean, she’d spend hours on the deck of research vessels, protected from the boiling heat by only a thin layer of sunblock, laughing as her colleagues dumped water over themselves in an effort to stay cool. “They’d just sort of stare at me,” Marsili remembers.
In the late 1990s, Marsili was introduced to a colleague named Anna Maria Aloisi, a physician and the director of the university’s pain clinic. Because Aloisi had access to a new high-tech lab, she volunteered to help Marsili with an experiment to test the impact of contaminants on swordfish and tuna. “A normal collaboration between scientists,” is how Aloisi describes it. “I had no idea how it would turn out.”
One of their early meetings took place on a cold day. Aloisi remembers a bitter wind blowing across campus. Marsili wore a short-sleeved dress. Her ankles were bare. “What are you doing?” Aloisi asked. “Don’t you feel the temperature?”
Marsili shrugged and shook her head. “It doesn’t bother me,” she said.
Aloisi told me, “I thought, OK, this may be some version of pain insensitivity. Not very common. Not super-rare, either.”
Normally, pain is our early warning system. We brush against a thorn and recoil before we’re cut too deeply. We put down a hot panhandle before we’re severely burned. If we get cold, we seek shelter. But people with a pain insensitivity disorder may not always realize they are seriously hurt until it’s too late. There have been cases of patients succumbing to heatstroke, frostbite or even bleeding to death; many die young from untreated injuries.
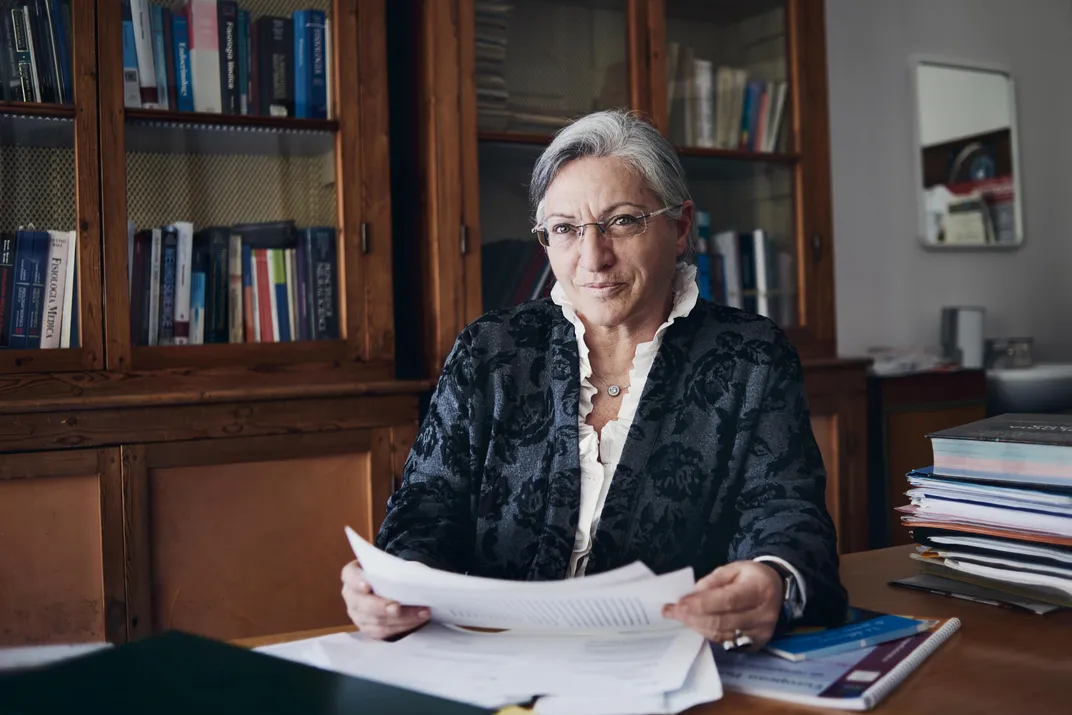
And yet the better Aloisi got to know Marsili, the more curious she became. At 33, Marsili was strong and healthy, and outside of the occasional tumble or kitchen accident, her condition—whatever it was—had not prevented her from living an active, physical life. She delighted in taking her two sons on rock- climbing trips; she loved to swim, to run, to chase her dog around the yard. And she showed no signs of intellectual disability, something often observed, for reasons not yet fully understood by scientists, in those with pain insensitivity disorders.
Then there was the important fact that Marsili did feel some pain, albeit in small amounts. Her early warning system, as it were, functioned just fine. (“My body tells me when something is wrong,” Marsili joked to me. “I just don’t always choose to listen.”)
As a researcher herself, Marsili understood Aloisi’s interest in her, and she told the physician, by now a friend, that she’d be happy to submit to a battery of tests, if Aloisi would be the one running them.
So Aloisi used a syringe to inject capsaicin, the chemical that gives chili peppers their heat, directly into Marsili’s forearm. Marsili reacted the way most of us would: She flinched, she shuddered, she screwed her face up into a tremendous grimace.
“Oh, Mama mia,” she recalls shouting. “What have you done to me?”
But after about a minute, Marsili’s features rearranged themselves. She slumped back into the chair. “Do you feel anything?” Aloisi asked, examining the syringe, which was still embedded in Marsili’s arm, feeding capsaicin into the skin. “No,” Marsili said.
“The way I’d put it,” Aloisi told me, “is that she was feeling the good pain, the pain that alerts us to danger. Then it disappeared. The bad kind of pain, the chronic pain, the ongoing pain that we take painkillers for—she simply didn’t feel that.”
She paused. “Extraordinary.”
* * *
Pain is one of our oldest evolutionary traits. It connects us to the outside world and modulates our interactions with it. But pain becomes a problem when its causes are mysterious, and when it persists beyond its usefulness in alerting us to danger—which, as anybody can tell you, happens all the time. We get headaches and bad knees; our backs start to hurt. One in five American adults, according to the Centers for Disease Control and Prevention, suffers from chronic pain, or pain unrelated to a recent injury and lasting longer than six months. The reason for the epidemic remains a matter of debate: It may stem in part from our modern lifestyles—less exercise, more processed food, more time in swivel chairs, craned over our desks—or it may be linked to the aging of the baby boomer generation. Or it may simply be that chronic pain has always existed, and we’re just talking about it more today.
Despite colossal amounts of study focused on understanding how pain works, though, in many ways the phenomenon remains enigmatic. We know that neurons throughout the nervous system send signals to the brain, which translates all that information into perception, but unlike senses such as touch, taste or smell, there is no single brain region responsible for the experience; there may be half a dozen or more. This has made treatment for pain an often-crude exercise, as the widespread prescription of opioids and the related epidemic tragically illustrates.
“You have a situation where the world’s population is aging rapidly, and more people are suffering from pain. And life expectancy is actually going down in the U.S. as a result of opioid abuse,” John Wood, the head of the sensory neurobiology group at University College London’s Wolfson Institute for Biomedical Research, told me this past winter. “So if you could find a solution to chronic pain that’s not addictive, not deadly, well, it would be greatly helpful, wouldn’t it? It would be a breakthrough of tremendous proportions.”
Wood, 68, is gregarious and rumpled, in a professorial kind of way; he wears his hair swept back from his head in an unruly, graying thatch. For more than three decades, Wood, a molecular neurobiologist, has devoted himself to understanding how the body processes pain, from both a physiological perspective and a genetic one. “A legend,” is how one of his colleagues described Wood to me. “You look at how many pain genes he’s been involved in studying and analyzing, and you realize just how much he’s changed the field.”
In the mid-2000s, Wood’s lab at University College partnered with a Cambridge University scientist named Geoff Woods on a pioneering research project centered on a group of related families—all from a clan known as the Qureshi biradari—in rural northern Pakistan. Woods had learned about the families accidentally: On the hunt for potential test subjects for a study on the brain abnormality microcephaly, he heard about a young street performer, a boy who routinely injured himself (walking across burning coals, stabbing himself with knives) for the entertainment of crowds. The boy was rumored to feel no pain at all, a trait he was said to share with other family members.
Woods was aware that the Wolfson Institute, John Wood’s lab, had recently published a paper on an inherited phenotype—essentially a collection of observable characteristics, such as eye color—that appeared to influence pain resistance. Perhaps, Woods theorized, the boy in Pakistan possessed the same phenotype. When Woods found the boy’s family, they told him that the boy had died from injuries sustained during a stunt leap from a rooftop. But several family members allowed Woods to collect blood samples, which researchers in England, using what was then cutting-edge software, scanned for genetic irregularities.
Sure enough, the Pakistani subjects all possessed the same abnormality Wood’s lab had documented: a subtle mutation in a gene regulating pain-sensing neurons, which disabled a key component known as Nav1.7. In a typical healthy adult, Nav1.7 helps notify the brain of pain or discomfort. When it’s removed or defective, no pain signal can be sent.
In 2006, with Woods as lead author, the scientists published their findings in the journal Nature. The reception was ecstatic. The work, one British reporter marveled at the time, “could lead to a safer range of pain-killing drugs.” Soon, several pharmaceutical companies unveiled plans to develop a drug to “block” Nav1.7. (Those efforts, though ongoing, have not yet panned out—scientists have had trouble getting the drug to cross the blood-brain barrier, where Nav1.7 does much of its work, among other challenges.)
Two years after the publication of the Nature paper, John Wood flew from London to Italy, to attend a pain conference sponsored by the University of Siena. There, he met Anna Maria Aloisi. “I remember Anna Maria telling me, ‘We’ve got this scientist here—she walks around in the winter in short dresses!’” Wood says. “And the whole story, it just got better and better as she went.”
Not only did Letizia Marsili possess an exceptionally high tolerance to pain, Aloisi explained to Wood, but so did much of her family. She’d done some rudimentary testing on Letizia’s mother, her sister, her sister’s daughter and Letizia’s own sons. All of them shared the same reaction to pain. In other words, Letizia’s pain resistance was not a random genetic one-off. It was inherited, as had been the case with the Pakistani clan.
Wood could hardly contain himself. “We were coming off the whole 1.7 discovery, which had profound implications for drug development,” he told me. “And now here was something equally promising.”

He asked if anyone at Siena had done any genetic mapping of the Marsilis. When Aloisi said nobody had, Wood requested new blood samples from as many family members as were willing to give them, and back in London, he summoned a young scientist named James Cox to his office. Cox, a self-described “gene hunter,” had played a crucial role in the research into Nav1.7 as a Cambridge postdoc. Now he was at University College, on a fellowship. Wood’s instructions to him were simple: Find the cause of the Marsilis’ pain resistance.
* * *
John Wood’s laboratory group works out of the Cruciform Building, an imposing, red-brick North London landmark that once served as University College’s hospital. On the day I visited, the halls were almost funereally hushed—you could hear an office door shut from dozens of yards away.
“The outside world does melt away a little here,” James Cox told me, grinning. As we walked, I asked Cox if he knew where exactly we were on the cruciform.
He put a finger on his stubbled chin, and pondered the question. “Goodness me,” he said. “Well, we’re on one of the wings, I know that. Bit of a maze, isn’t it?”
I followed him into his lab, a harshly lit space dominated by banks of computers and incubators full of petri dishes teeming with live cells. Cox recalled that when he first started his career as a gene hunter, the task of locating mutations had been “tedious.” But in the years since the human genome was sequenced and computerized, the rise of what’s known as exome analysis has allowed for rapid work-ups of a person’s genetics, by focusing only on the protein-coding portions of genes.
Once Cox and his colleagues sequence a subject’s DNA, a process that takes a couple of weeks, they embark on a lengthy game of cat and mouse. In the case of the Marsili family, the first phase was led by a geneticist and bioinformatics specialist at University College named Jose Bras, who analyzed the genomic data with specialized software such as the Genome Analysis Toolkit and his own custom-built programs. The software allowed Bras and Cox to measure the Marsilis’ genomes against databases of genetic control sets of people who perceive pain normally, in order to isolate novel genetic variants. Dozens of genes stood out—not unusual, considering that humans possess more than 20,000 of them. “Sometimes the gene jumps out of the list, sometimes it doesn’t,” Cox told me. The team got to work examining how each one worked.
In 2012, Cox spotted a mutation in NLRX1, a gene that appears to support the central nervous system. It seemed a promising candidate. But to be sure, Cox devised a test, cloning the “wild-type” version of the gene (essentially a control) and the mutant version present in the Marsilis’ genetic code. They were looking to see how the two genes produced proteins in lab-grown cells; if the proteins behaved the same way, NLRX1 was probably not responsible for the Marsilis’ condition. If the mutant protein was defective, however, they had likely identified their culprit.
Eighteen months later, Cox was finding that no matter how many tests they devised, the proteins always behaved the same way; NLRX1, in other words, was a bust. By the time the NLRX1 mutation appeared in updated genome databases, which meant it had shown up in people who felt pain normally, Cox says they were relieved—it meant they weren’t crazy. “We sure as hell couldn’t prove it was pathogenic!” he told me.
Still, it was back to the drawing board. Cox tried not to let his frustration get the best of him. Years earlier, he had been part of a group that sought to unpack the role genetics can play in learning disabilities, and he’d grown to accept the highs and lows that come with searching for the equivalent of a needle in a haystack. “Because when you do find a gene, you’re able to tell a family, ‘This is why you feel this way,’” Cox told me. “It’s incredibly rewarding.”
* * *
The Marsilis did not visit London while James Cox was conducting his research. They didn’t need to—the quantities of blood they’d provided had been enough. Meanwhile, they moved on with their lives: Letizia’s sons graduated from high school. One pursued his love of soccer, playing the sport semi-professionally (Ludovico was, perhaps not surprisingly, a battering ram on the pitch); the other, Bernardo, opened a small grocery store inside Siena’s cobbled old town.
But Cox didn’t give up on the search. In 2014, after sequencing the Marsilis for a third time with the latest technology, and focusing only on coding genes, he and his team were left with just two novel variants in the family’s shared phenotype. Suddenly, a mutation in a gene known as ZFHX2, which affects neurons that play a role in transmitting pain signals to the brain, seemed like it might hold the key to their condition. This time, experimentation showed that the mutant protein behaved differently from its wild-type counterpart.
The next step was to reproduce the mutation in a living creature. John Wood is a specialist in rodents bred to lack a specific gene or phenotype or to include rare mutations. “The easiest way to explain it,” Wood told me, “is that you manipulate the cells genetically, you inject them in a pseudo-pregnant mouse, and make a baby mouse. You wait for a bit, and one day, a young mouse arrives at the lab in a box.”
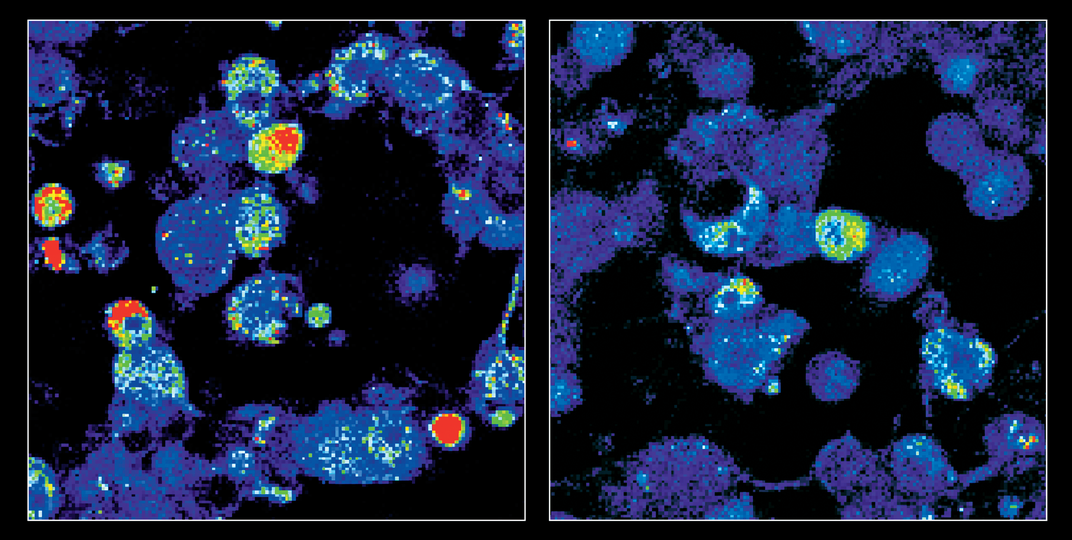
In early 2015, a batch of mice engineered to lack ZFHX2 arrived at the UCL lab, where they were put through a series of pain threshold tests. The researchers used two different methods, which would serve as a proxy for pain under Britain’s animal-testing regulations: One applied gradually increasing pressure to the mice’s tails; the other test involved miniature hot plates. “It’s just a latency thing,” Cox told me. “It’s like if you put your hand on a radiator—how long does it take for you to move?”
The mice missing the ZFHX2 gene had remarkable reactions: They showed higher pain thresholds for applied pressure to their tails, but some were extra sensitive, rather than less sensitive, to heat—the opposite of what the scientists expected. Still, the experiment seemed to show that ZFHX2 played an important role in regulating pain, even if they hadn’t yet figured out how. “So we went at it again,” Cox recalled. This time they ordered mice with copies of the precise ZFHX2 mutation observed in the Marsilis’ genetic code.
Several months later, the second batch of mice were put through the same tests as the first. This time, the animals’ reaction to the hot plates was consistent—they were significantly less sensitive to heat. They seemed to tolerate it, in the same way the Marsilis did.
Six years after he’d embarked on his quest, Cox had found the right gene. “You always tell yourself to not get too excited,” Cox recalled, “but it is impossible not to.”
In late 2017, Cox published his findings in the journal Brain, noting that the mutation to the ZFHX2 gene, now known as Marsili syndrome, was extremely rare or even unique. As far as he could tell, only the members of one small family in Tuscany possessed it.
The broad significance of their analysis is that it showed that ZFHX2 was crucially involved in pain perception in a way nobody had previously understood. Unlike more frequently documented cases of pain insensitivity, for instance, the Marsili family’s mutation didn’t prevent the development of pain-sensing neurons; those were still there in typical numbers. Yet it was also different from the Pakistani family’s mutation, whose genetic anomaly disabled a single function in pain-sensing neurons. Rather, ZFHX2 appeared to regulate how other genes operated, including several genes already linked to pain processing and active throughout the nervous system, including in the brain—a sort of “master regulator,” in the words of Alexander Chesler, a neurobiologist specializing in the sensory nervous system at the National Institutes of Health, in Bethesda, Maryland, who was not involved in the study.
“What’s so exciting is that this is a completely different class of pain insensitivity,” Chesler says. “It tells you that this particular pathway is important in humans. And that’s what gets people in the industry excited. It suggests that there are changes that could be made to somebody to make them insensitive to chronic pain.”
* * *
After Cox and his colleagues published the paper, the Marsilis began to receive new visitors: Every week, it seemed, a television crew arrived at their door. The producers came from Austria, from Brazil, from across Asia. The Marsilis found themselves participating in circuslike stunts, such as submerging their bare hands in bowls of ice.
Last December Letizia Marsili showed me one of the more outlandish television segments that arose from those visits—a 26-minute documentary made by filmmakers in Japan, in which events from Letizia’s life were dramatized, with Japanese actors playing the roles of the Italians.
“It makes you laugh, doesn’t it?” she said, closing her laptop. We were sitting in the living room of her home, in a former convent perched on a hill not far from the gates of the old town. Through the back window, I could see across a corrugated landscape of farmland and copses of cypress trees. The Marsilis’ dog, Prince, scuttled back and forth over the parquet floor, before settling into a nest of blankets on the couch.
I asked Letizia if she ever felt uncomfortable being viewed as a guinea pig—a scientific oddity. She recalled an invitation to appear on a popular news show, which she hoped would provide a scientific discussion. She arrived to find the screens in the studio filled with images of female superheroes. She tried to crack a joke: “I did fly here today,” she said to the host.
But that appearance was an outlier. “Generally, I’ve been able to communicate to people that behind the guinea pig there’s this amazing research,” she told me. And if it meant she had to stick her hand in ice once in a while—or take time away from her own academic work to sit down with an American journalist—so be it. “To me,” Marsili went on, “the most important thing is taking our condition and making something good of it.”
What form that good might take is something scientists are wrestling with. One possibility is a drug that would block, in some way, the function of one of the pain-signaling genes regulated by ZFHX2, or a suite of them, as researchers learn more about how the ZFHX2 mutation controls the larger process of allowing some pain signals through while keeping a limit on chronic pain. But the identification of a single gene that seems to play such an important role in pain processing makes it a particularly attractive target for gene therapy itself.
By experimenting with the function of ZFHX2, “You might be able to ‘turn up’ or ‘turn down’ a number of genes involved in pain,” says Chesler, of NIH. “If you find something that’s regulating a lot of genes, you could have one target but many effectors—and there’s something really appealing about that.”
In other words, there is a scenario, as the science improves, in which a person suffering from chronic pain might have his or her genetic code altered to mimic that of the Marsilis. Already, Cox’s group at UCL has shown that such a process is possible in cells. “There are the technical challenges, and the ethical ones,” Cox told me. But Cox and Wood are optimistic. “If we get really strong evidence, we can try things in proof-of-concept studies”—human trials, in other words. “So it is an exciting idea. And the potential is there.”
* * *
One afternoon, I was at the Marsilis’ home in Siena when Letizia’s mother, Maria, and her father, Ugo, dropped by. Maria is 80, but strong and hardy; she is smaller than her eldest daughter, and less angular, but the two share the same wry smile. “Until all the research came out,” Maria joked, “I thought I was just very, very strong.”
She had the same sorts of stories as Letizia: The kitchen accidents, the fall on an escalator that she learned broke her ankle only after her grandson convinced her to see a doctor. “I’ve done a lot of thinking about it,” she told me, “and I believe that if this was inherited, it did not come from my mother. She definitely felt pain, and told us all about it!”
Later, I dropped in on Bernardo Marsili’s grocery, not far from the 335-foot tower that looms over Siena’s historic district. The shelves were stacked high with specialty cheeses and wines; behind a glass sneeze guard Bernardo had positioned dozens of slabs of cured meat. “It was always my dream to open a place like this,” he told me. And now you’re famous, I said. “Free publicity!” he agreed.
Bernardo, 22, does not yet have children of his own, but he told me he’d be pleased if they inherited his family syndrome. “You know, my friends sometimes tease me, joke with me,” he said. “And yeah, I have to be a little more careful than other people. But it’s also something that’s special, what we have. It’s something that could change the world.” He smiled. “And something I’d want to share.”
:focal(3837x1290:3838x1291)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/4d/74/4d745020-a11f-4638-a08c-c5168b2830d2/may2019_g04_pain.jpg)