A year ago, when spring rains made their way through the Southwest and the frozen earth began to warm, the first cases of Covid-19 appeared in Navajo Nation. Though sparsely populated, with 172,000 residents in a region the size of West Virginia, Navajo Nation was particularly susceptible to the pandemic because of systemic poverty, chronic food insecurity and overall poor health. The tribe has faced such high infection and death rates—at least 975 people have died of Covid-19—that the federal government set aside $714 million in aid to the Diné people, as we are called in our native language. But perhaps the most noteworthy response to the onslaught of disease has been the work of courageous caregivers—including the five physicians pictured here, all from traditional Diné families and all quick to rise to the historic challenge.
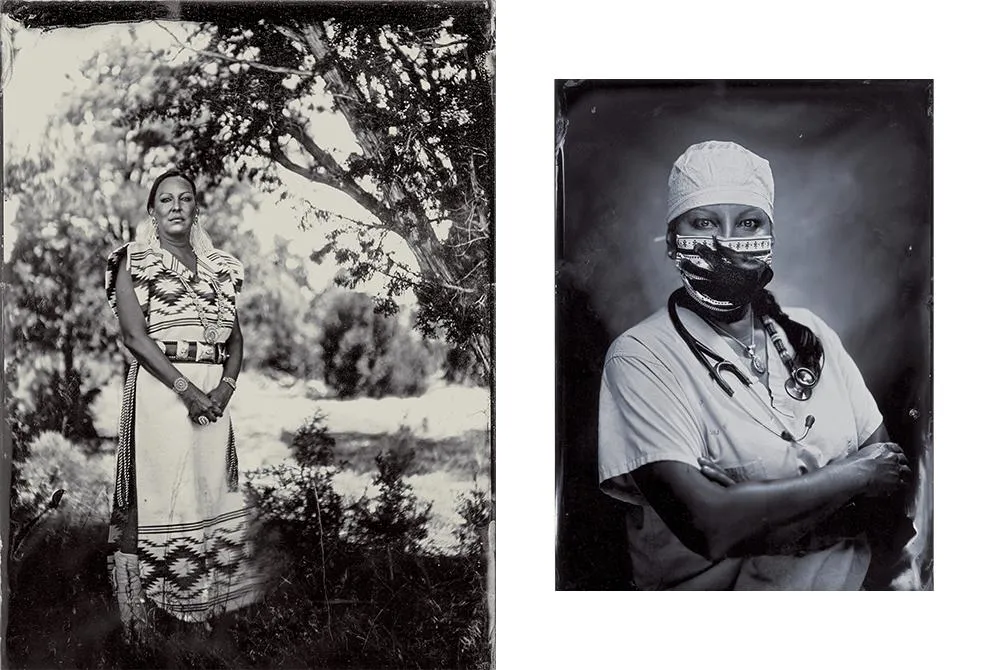
OB-GYN, 18 years
Tuba City Regional Health Care Corp., Arizona
Jennifer Whitehair wears a traditional Navajo rug dress and sash woven by her paternal aunt; another aunt gave her these slippers when she graduated from medical school in 2002. In her scrubs photo, Whitehair is wearing a face mask that represents the missing and murdered indigenous women’s movement; Whitehair hand-beaded the stethoscope herself. “The Navajo are resilient,” she says, “and their strength in times of turmoil will pull them closer together after this is all over.” Eric Retterbush
“In the blink of an eye, community tents went up, red triage tents went up and we had to cancel all our elective surgeries,” says Vanessa Jensen, a surgeon in Fort Defiance, Arizona.
Michelle Tom, a physician working in Winslow, Arizona, began doing “car triage” for Diné patients, a drive-through arrangement for testing patients quickly and safely.
Navajo Nation has always lacked adequate infrastructure to meet residents’ needs, even compared with other rural areas. This deficiency stems from the federal Army’s push in the mid-1800s to conquer Navajo lands and forcibly relocate the Diné to reservations. In a territory spanning 27,000 square miles across Arizona, Utah and New Mexico, there are only 13 grocery stores. Around 15,000 homes lack access to electricity. About one in three families must haul water to their homes every day. Scant health care facilities—400 or fewer hospital beds—and shortages of medical equipment, including ventilators, have also made it tough to cope with Covid-19.
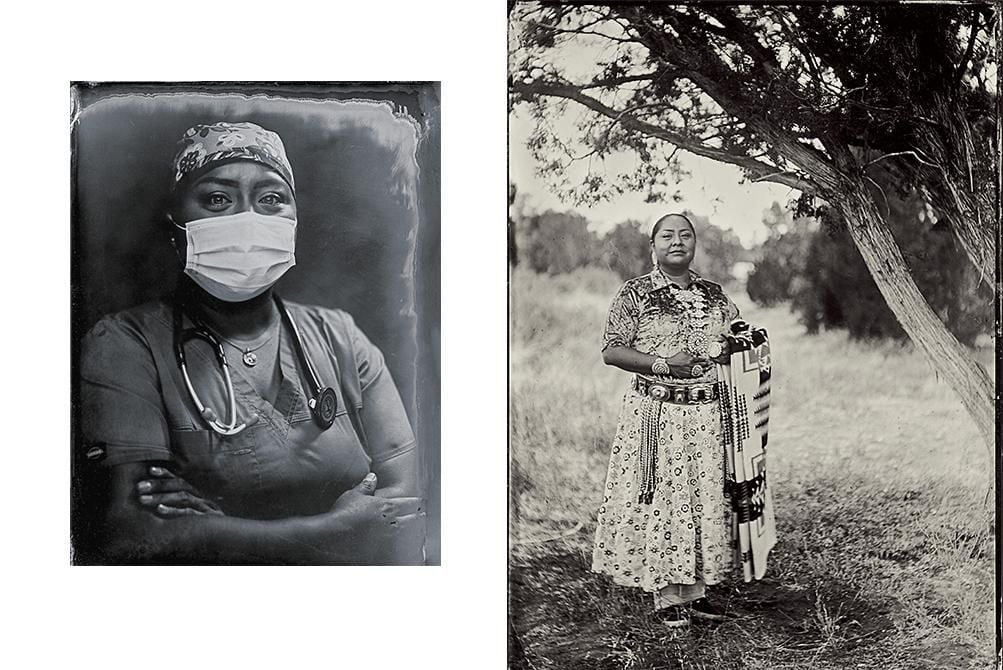
Deputy Chief of Staff, 9 years
Tuba City Regional Health Care Corp., Arizona
“I work in the same hospital that I was born in,” Calderon says, “with many colleagues who were my own doctors when I was a kid.” Her traditional outfit includes a squash blossom necklace and moccasins passed down from her grandmother. “Getting dressed is a huge chore, involving tightening the sash belt and tying the moccasins and tying my hair into a traditional bun.” Eric Retterbush
“On the Navajo reservation, we have unique social issues that are extremely challenging that the rest of the world may not completely understand,” said Jennifer Whitehair, an obstetrician-gynecologist working with Native patients in Tuba City, Arizona. “I think they would find it difficult to believe that these living conditions could exist in a non-third-world country.”
Tom, who specializes in family medicine, collaborated with locals to distribute supplies such as personal protective equipment, water and other basic necessities to community members. Appearing on “NBC News” in April, she detailed the dire needs of her patients and colleagues; people responded by sending hundreds of thousands of dollars, masks, gloves, face shields, water and nonperishable foods. Tom worked with an existing nonprofit, United Natives, to handle the donations, and found warehouse space to store the supplies. The group spent about $120,000 just on disinfectant sprays and wipes. “A lot of elders sent me their stimulus checks,” Tom says, “but I couldn’t bring myself to [take their donations]—I ended up sending those back because I felt they needed it.”
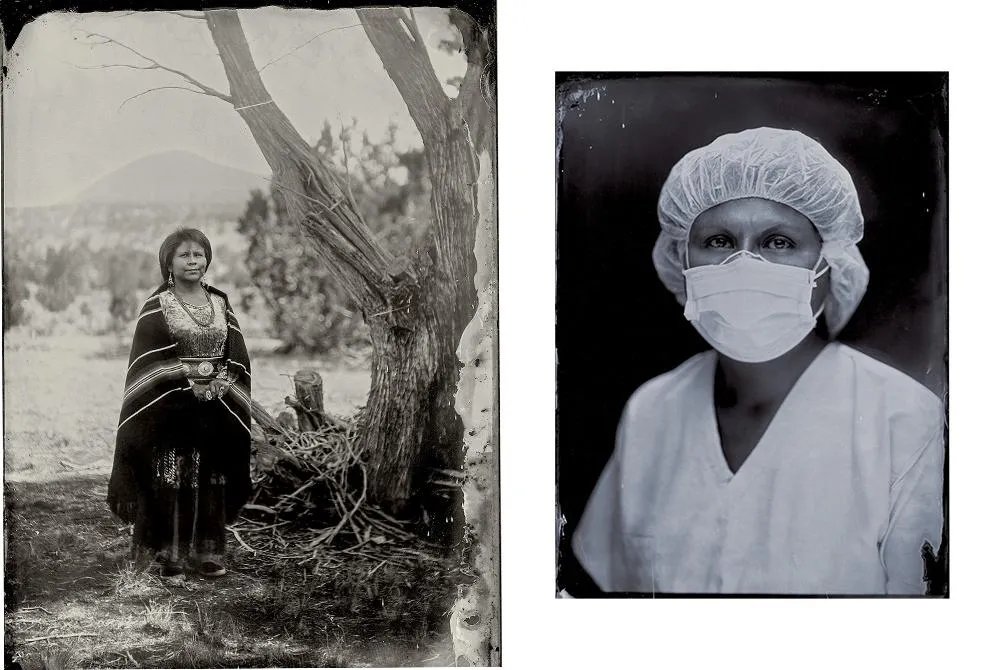
Internal medicine, 12 years
Northern Navajo Medical Center, New Mexico
LaWanda Jim lives in Upper Fruitland, New Mexico, a farming community in Navajo Nation. Her ceremonial dress includes a silver concho belt, which her mother gave her when she graduated from high school, and turquoise bracelets, a gift from her father when she graduated from the University of New Mexico School of Medicine in 2008. Diné culture offers inspiration and solace, Jim says: “Our stories tell us of previous times when we dealt with monsters and how we survived and overcame them.” Eric Retterbush
Whitehair recalls her first Covid patient. “The patient was Covid-positive at 37 weeks pregnant, febrile with severe shortness of breath. I was still really scared because all I had seen was death at this point, and interacting with a Covid-positive patient felt like a potential death sentence for all of us health care workers.” She goes on, “I was very afraid of bringing this home to my family, especially my father, who is Navajo and has other health co-morbidities.” Still, Whitehair persevered. “I put on all my personal protective gear and went to the hospital to see her. She was too sick to stay at our rural hospital but ended up getting transported to a higher level of care. She delivered a healthy baby and did extremely well after getting better.”
With about half of adults on Navajo Nation afflicted by Type 2 diabetes or prediabetes, physicians worry that Covid concerns are leading some to overlook other medical risks. “A lot of patients got so scared and forgot to take care of themselves and forgot to take care of their diabetes,” says Sophina Calderon, a doctor at Tuba City Regional Health Care Corporation in Arizona.
Like most indigenous cultures, Diné people are deeply rooted in their community. Family, clanship, or as we say, K’é (kinship), is a fundamental value, helping us understand who we are. The pandemic has threatened that part of life. “Navajo families are large,” says LaWanda Jim, a physician who practices in Shiprock, New Mexico. “I have 60 first cousins and numerous aunts and uncles, and we miss one another during the pandemic. It wasn’t unheard of to gather year-round to celebrate weddings, graduations and ceremonies. My family is involved in summer and winter ceremonies. My son dances in the winter ceremonies. When we’re not able to gather the way we do, it weighs heavy because that was a resource for maintaining our resilience.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/e9/aa/e9aa49b0-7e45-451f-a1a1-6b43d8c0fa66/vanessajensen.jpg)
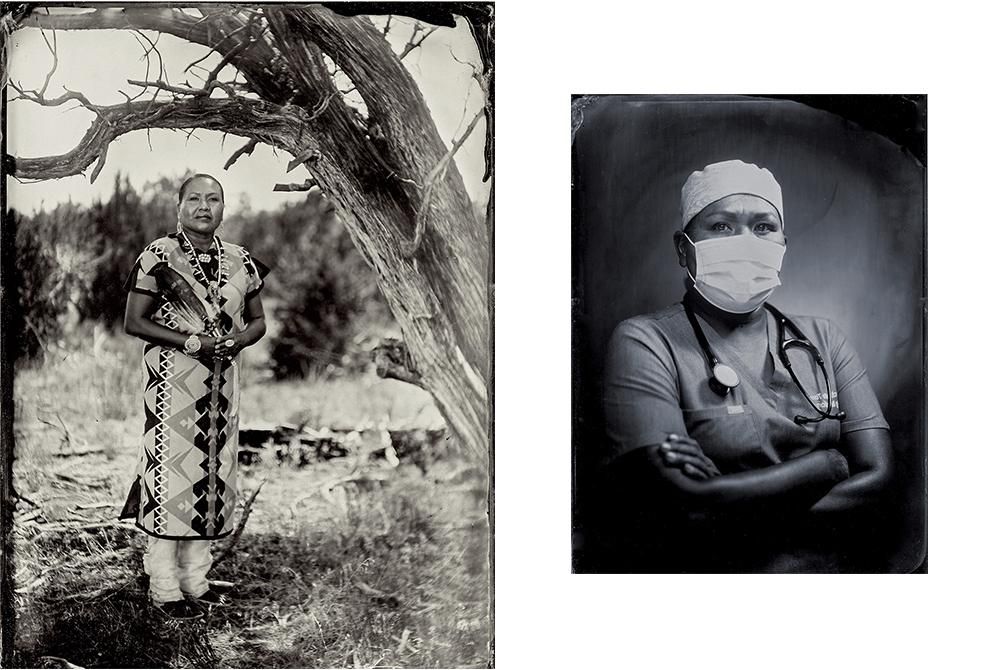
General surgeon, practicing 17 years
Fort Defiance, Arizona
Right, Jensen stands near San Francisco Peaks, a mountain range in north central Arizona sacred to the Diné people. For this portrait, she wears a black velveteen dress, turquoise jewelry borrowed from female family members and moccasins made by a cousin. "I dressed and prepared myself as if I were going to pray for healing and armored myself for this task with blessings," Jensen says. Her community ties, she says, build trust. "Patients know [my] family, they know my dad's side, they know my mom's side, they know my clan." Eric Retterbush
As a result, Jim says, “I’ve had to think about, ‘How do we do this? How do we acknowledge our relationships and keep those relationships strong despite social distancing, wearing masks, not being able to shake hands, say Yá’át’ééh [hello]?’”
At the core of Diné culture is Hózhó, a philosophy of harmony, beauty and mental and spiritual wellness; more broadly, Hózhó refers to a way of walking this earth that is inherently good. Diné physicians have integrated Hózhó into medical care. Some clinics offer spaces where people can pray with traditional medicines, while others have hired traditional practitioners to support patients.
“Being Diné and working with a lot of patients who rely heavily on traditional medicine, I went about trying to work with medicine men to formulate a safe plan,” says Calderon. With her colleagues, she developed new ways to hold traditional healing and prayers, like phone calls or Zoom meetings.
Family medicine, 5 years
Winslow Indian Health Care Center, Winslow, Arizona
“In our Navajo belief system, it’s always about your community,” Tom says. “You’re only as strong as your family. You have this need to make a better place for our grandchildren. I always felt like it was my calling to be a healer.” A former basketball star at Arizona State University, she’s wearing a traditional Navajo rug dress as well as a squash blossom necklace made by her mother. The eagle feather, often wielded by traditional Diné medical practitioners, was a gift from her uncle. Eric Retterbush
In November, like many communities around the country, Navajo Nation saw a new surge in cases, with the positivity rate soaring to 37.8 percent on November 20. But in December, vaccines brought new hope—and Tom says she and her staff are better prepared with every passing day. “Before, there was a lot of fear. Now, I know what to say to patients, I know what I’m looking for, and I can give my patients better answers so they feel more comfortable. Things are a lot better, the mental health of my colleagues is better, and the work is more manageable: mentally, physically and even spiritually.”
:focal(282x71:283x72)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/bf/74/bf748919-a015-4ba5-a3eb-73e8a84a64e1/michelle-tom-mobile.jpg)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/90/67/9067d1a8-37f9-4f0a-b30f-3c2adaaeadb2/navdocopemer.jpg)