How Do Scientists Measure the Public Health Impacts of Natural Disasters?
In the wake of this year’s hurricanes, epidemiologists are assessing the effects of mold, toxic leaks and other threats
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/e5/2a/e52ae130-32cc-49bd-a379-26290a5f3f31/file-20171017-19058-1vmpwto.jpg)
Two months after Hurricane Harvey submerged much of metropolitan Houston, recovery is under way across the city. Residents and volunteers are gutting and restoring flooded homes. Government agencies and nonprofit organizations are announcing cleanup programs and developing plans to distribute relief funds.
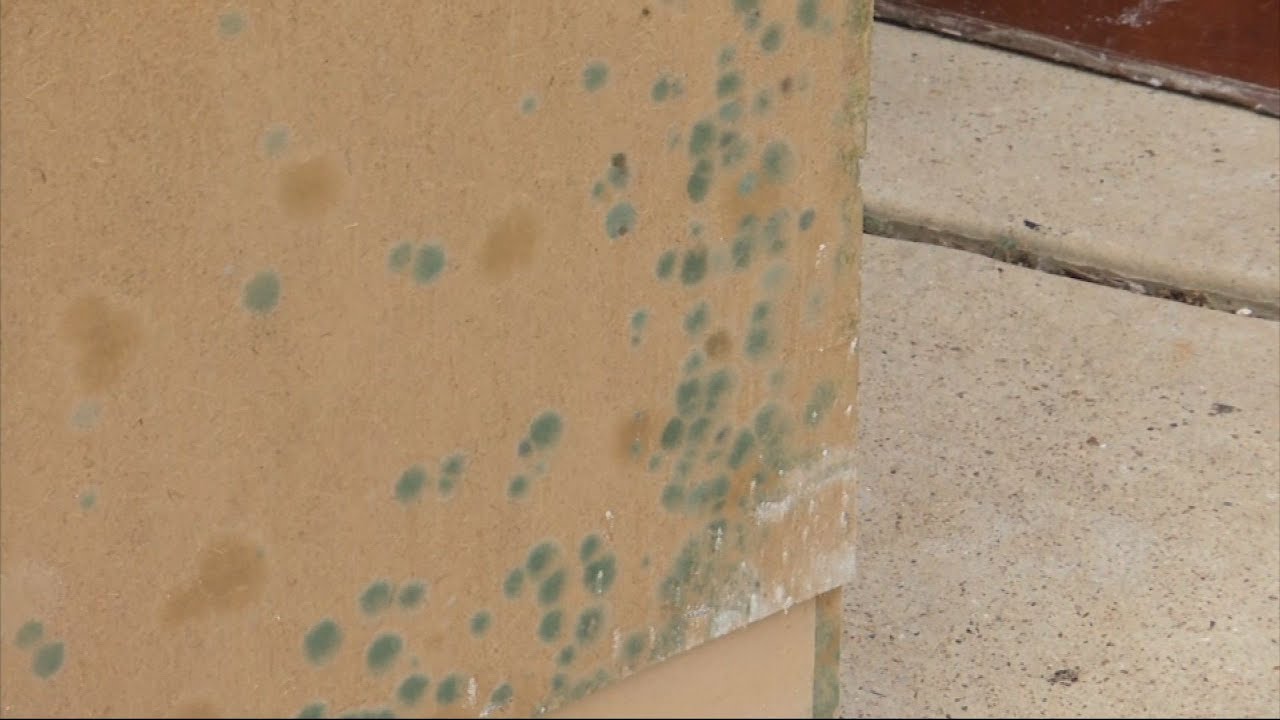
But many questions remain about impacts on public health. What contaminants did floodwaters leave behind? How many people are being exposed to mold – which can grow rapidly in damp, humid conditions – as they repair their homes? Will there be an increase in Zika, West Nile or other vector-borne diseases as mosquito populations recover? Or an uptick in reported cases of other illnesses?
I am an epidemiologist, and my work focuses on understanding the causes and distribution of illnesses, injuries and deaths among different populations – a critical issue during and after major disasters. Our work starts when the water recedes: We want to find out how well residents were prepared before the storm, and what kinds of health impacts they may be experiencing now or can expect in the future. If they still have unmet needs, we can connect them with information and resources.
Researchers are at work across Texas in areas impacted by Harvey. Here’s what some of us are doing.
Contaminants left behind
I’m currently working in Houston with partners from community organizations including Texas Environmental Justice Advocacy Services and the Houston Health Department to sample soil and sediment that was mobilized by flooding during Harvey.
For example, residents of Manchester, a neighborhood in Houston’s East End with many low-income and minority residents, live close to industrial sites, refineries and chemical storage facilities, many of which were flooded during Harvey. They are worried that contaminated sediments may have been washed into their yards and could threaten their health if dust enters homes as it dries. This is a valid fear. A 1999 study found that dredging in New Bedford, Massachusetts mobilized toxic PCBs from harbor sediments, which later were detected in house dust and yard soil in nearby homes.
We also are working around Buffalo Bayou, a slow-moving river that flows through Houston and buffers the city against flooding. Buffalo Bayou is surrounded by public recreation areas, including nature trails, bike paths, children’s playgrounds and dog parks. Today trails in some of these parks are covered by up to six feet of accumulated sediment. We are working with the Houston Health Department to collect and test these sediments for environmental and health hazards.

Documenting contamination is only the first step. Residents, the media and public officials can easily misinterpret lab results and risk predictions, which are based on complex modeling.
To help people understand what these exposures could mean to their short-term and long-term health, we are working with established teams of toxicologists, environmental health specialists, civil engineers, chemists, risk communication specialists and graphic designers as part of Texas A&M’s Institute for Sustainable Communities. We are also exploring ways to use social media to communicate with residents at risk as part of the university’s new Superfund Research Program.
During and after Harvey, some Houston residents were exposed to complex mixtures of contaminants from chemical plants and toxic waste sites. We need better, more accessible materials and communication tools to help people understand what kinds of health risks they may face if they have come in contact with industrial chemicals or hazardous waste.
New data sources
After major disasters, epidemiologists need ways to determine quickly where the greatest needs lie. Student volunteers from my EpiAssist program have helped conduct surveys to rapidly estimate remaining unmet needs and assess how prepared residents were when the storm hit.
We also can measure people’s needs by looking at how they use telecommunications. After Hurricanes Katrina and Rita in 2005, researchers at Texas A&M’s Department of Landscape Architecture and Urban Planning analyzed use of 2-1-1, a telephone number that Texas used to help Katrina evacuees in Texas to search for services across the state. By studying 2-1-1 data, they were able to identify unmet needs in real time.
Now people are using social media networks and apps during disasters. After Harvey, many desperate flooding victims turned to Facebook and Twitter to appeal for help or find supplies. With colleagues from Texas A&M’s Computer Science and Engineering and Health Promotion and Community Health Sciences departments, I am analyzing tweets sent during Harvey to see how volunteer responders provided lifesaving assistance, and to understand risks and exposures that many volunteers may have experienced.
Encouraging update posted on our Facebook page this morning! https://t.co/pSLJi9n9Tj. pic.twitter.com/y5SYdjgOsW
— Insulin for Life USA (@Insulin4LifeUSA) September 2, 2017
Long-term questions
More information about Harvey’s impacts will become available over time and can tell us a lot. I will be requesting and analyzing data from the Federal Emergency Management Agency to design studies to assess the quality and pace of recovery.
One key priority should be to enroll a large number of Houstonians in a cohort study that can follow them over time to see how strongly certain risk factors – such as exposures to contaminated flood waters, chemical spills or leaking Superfund sites – are associated with future illness. Researchers track cohort members’ health by surveying them periodically, collecting biological samples from them and reviewing their medical records.
Studies like this after past disasters have produced important findings. Researchers used a registry of firefighters and emergency responders who were involved in the Sept. 11, 2001 terrorist attacks to identify cancers from exposure to ignited chemicals and materials. The National Institute for Environmental Health Sciences created a similar registry after the 2010 Deepwater Horizon oil spill to assess health outcomes of people who were involved in cleanup and remediation activities.
An emerging field
Epidemiology is more than 150 years old, but applying it in disaster settings is relatively new. Using epidemiologic methods and study designs in post-disaster settings can help identify vulnerable populations, quantify deaths and injuries and determine how disasters have affected public health. It also can lead to better decision-making and use of resources.
Wide-scale disasters can create conditions that foster serious health threats afterward. For example, in Texas and Florida communities that experienced hurricane flooding and where Zika virus is endemic, health officials may need to pay closer attention to people of childbearing age in shelters and put more resources into mosquito control and personal protective measures. Officials in Puerto Rico have reported two confirmed and 10 suspected cases of leptospirosis, a disease transmitted via contaminated water, in the wake of Hurricane Maria. Amassing more evidence about how disasters affect health will improve readiness, response, recovery and mitigation for all Americans.
This article was originally published on The Conversation.
Jennifer Horney, Associate Professor of Epidemiology and Biostatictics, Texas A&M University