It was January in New York City, drizzly and gray. At the northwest corner of Manhattan, through the arched doorway of Columbia University’s Mailman School of Public Health, a virologist named Simon Anthony was writing a grant proposal, asking agencies to fund his work on a family of pathogens called coronaviruses. These viruses—named for their crownlike arrays of spiky outer proteins—had caused the worldwide SARS epidemic in 2003, and another epidemic called MERS that began in 2012.
For more than a decade, Anthony had been discovering new viruses, trying to understand which changes in their makeup transformed them from quiescent inhabitants of bats to ferocious threats to human beings. He’d also been reading the news, and almost as an afterthought, he added a sentence to his grant proposal: At that moment, he said, China was reporting that one person had died from an infection caused by a coronavirus that had never been reported before.
The next day, he was reading the news on his phone as he walked the six blocks between his apartment and his lab, and learned that there had been more than one death. He changed the number in his proposal. A day later, he had to change it again. “Over the course of a week, the deaths went up, and up, and then they jumped up,” he recalled to me. “And there was a moment when I thought, Oh my God. This really could be it. The thing we’ve been talking about for the last ten years.”

Anthony, who is an assistant professor at Columbia’s Center for Infection and Immunity, has long been aware that the animal world is teeming with pathogens our immune systems have never experienced—and that one of these might trickle unnoticed into the human world and spark a conflagration. But Anthony is also part of a small, influential cadre of researchers who believe that such epidemics can be prevented—if viruses can be detected before they make the fatal leap.
* * *
Almost two-thirds of human diseases originate in animals. Measles, first described in the ninth century, is thought to have come from cattle. HIV most likely leapt into our world via monkeys and apes in the 20th century. The most terrifying epidemics of the past generation—West Nile virus, SARS, MERS, Ebola—began when an animal pathogen found its way into a human.
Once or twice a year, a “spillover” of an animal pathogen into people ignites a new infectious human disease. It’s possible there are many more such eruptions in which an animal pathogen flares briefly to life in one or several people and then dies out—either because the virus isn’t well adapted for human spread, or because the infected people live in isolated places and don’t have high levels of contact with others. By one estimate, there are more than 827,000 viruses in the animal world that have the potential to infect humans. We encourage these spillovers whenever we cut roads through the wilderness, clear forests to grow crops, catch wildlife to sell as trophies or butcher for food, or pen chickens and swine in places where bats and wild birds can mingle with them.
One spillover that caused international alarm at the time was the H5N1 avian influenza. It jumped to humans from poultry sold alive in Hong Kong markets in 1997, infecting 18 people and killing six. Hong Kong squelched the outbreak by killing every one of the 1.3 million chickens in the territory. But in 2004, a new strain of the H5N1 virus spread outward from Southeast Asia. By the end of 2005, it had sickened 142 people as far west as Romania, killing more than half of them, and prompted the slaughter of millions of birds.
The global spread of bird flu—and the agricultural destruction it wrought—made a deep impression on a federal infectious-disease specialist named Dennis Carroll. Carroll worked at the U.S. Agency for International Development (USAID). Until that point, most of his work on outbreaks—malaria, tuberculosis, river blindness—had involved teaming up with national ministries of health. The H5N1 flu made him see what such partnerships missed. “If you’re concerned about a virus killing off people, but it’s principally circulating in poultry, you don’t go to the public health or medical professionals,” he says. “You go to the veterinarians.”

Carroll started working with animal-health experts across the developing world, who taught farmers and live-animal sellers how to reduce exposures and risks. The effort did what the agency had hoped: It suppressed the spread of the H5N1 bird flu, forcing it back from more than 50 countries into just a few.
But H5N1 wasn’t gone yet. The virus inhabits wild waterfowl, which pass it to domesticated and wild birds as they migrate across the world. This made Carroll wonder: What if someone had pinpointed which groups of wild birds carried the virus? Could farmers along those migratory routes have been persuaded to alter their methods—for instance, raising their chickens in closed sheds? More broadly, could detecting pathogens before they spilled over from the wild help humans prevent the next pandemic?
So Carroll created a project called Predict, a coalition of the Smithsonian Conservation Biology Institute, the One Health Institute at the University of California at Davis, the EcoHealth Alliance and the Wildlife Conservation Society (both in New York City) and the San Francisco risk-modeling firm Metabiota. The five organizations had all been working at the intersection of animal science, conservation and human health. Under Carroll’s leadership, the coalition applied for USAID funding, and received the first grant to launch their work in 2009.
“I really credit Dennis,” says Jonna Mazet, a veterinarian who directs the UC Davis One Health Institute and served as Predict’s principal investigator. “At the time it was disputed whether emerging infectious diseases really were one of the world’s biggest problems. Now everyone knows that.”
* * *
Finding viruses in the wild is hot, messy, risky work. The scientists working with Predict work with local governments and nonprofits to pinpoint the places where those animals’ worlds intersect most with human society. Then they go out into the field to collect samples, without confining or killing the animals.
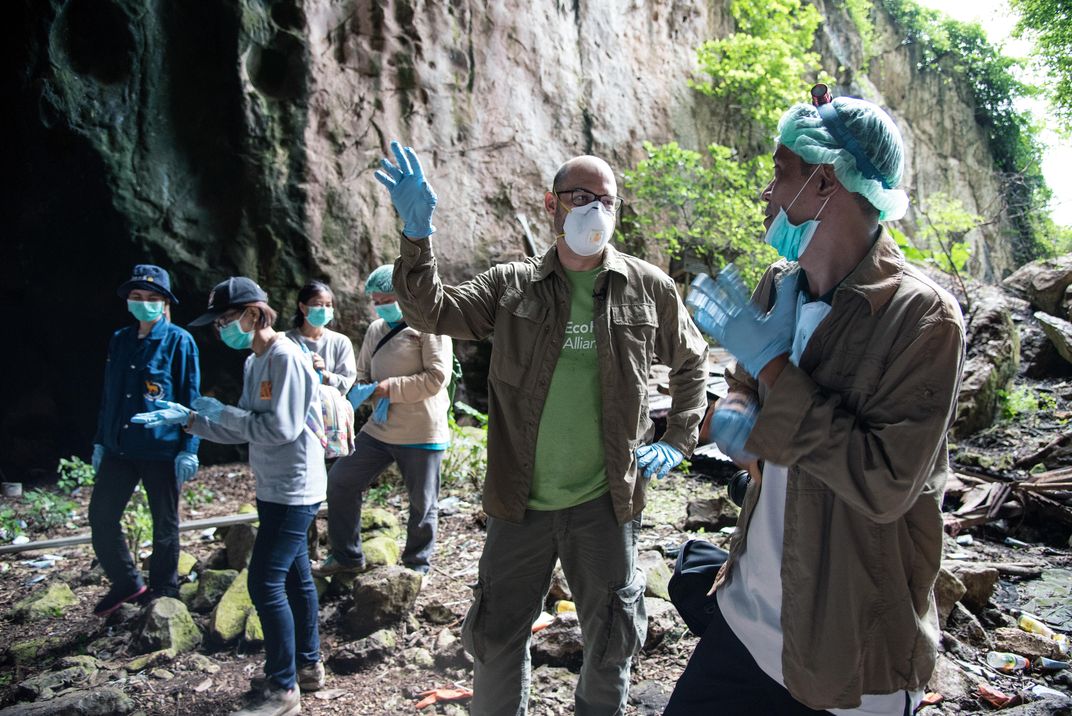
Between May 2016 and August 2018, for instance, researchers working with Smithsonian’s National Zoo looked for novel viruses in bats in Myanmar. They spent muggy nights trooping through jungles in personal protective gear: Tyvek suits and footwear covers, gloves and masks and aprons, head lamps and face shields. Sometimes they scooped bat feces and urine from tarps they’d laid by crawling into caves where bats nest during the day. Other times they caught bats in mist nets—long, loose nets of ultra-fine filaments that they had strung between poles before the sun went down. The researchers disentangled the bats, took blood samples from their veins, swabbed their mouths and rectums—being careful not to get bitten—and then let the animals go, unharmed.
During the day, the teams spoke to people who lived nearby, asking about their everyday habits—farming, trapping, forestry. With permission, they acquired samples from these humans as well, to look for evidence—immunologic signals in blood, for instance—that viruses found locally might already have jumped to humans without being recognized.
Working this way in 31 countries over the course of ten years, Predict collected samples from more than 164,000 animals and people. Each sample was split and frozen. One portion remained at labs in the home country, where scientists tested it for viruses and kept it as a form of national intellectual property. When those labs found something worth scrutinizing further, the other portion came back to the United States, to labs including Anthony’s.

Anthony is originally from Britain, but after finishing his PhD at Oxford in 2007, he took a post-doctoral position at the San Diego Zoo’s Institute for Conservation Research, studying wildlife diseases. This put him in California’s conservation and virology community at a key moment, just as Predict was coming together. He began talking to researchers in Davis and San Francisco, and when he moved to his current position at Columbia, he started working for Predict from New York. He now serves as one of two U.S. leaders on Predict’s laboratory side. (The other is at UC Davis.)
Here is how his role works: The samples that come from the field, frozen to minus-80 degrees Celsius, contain a chaotic mix of materials: cells from the bats’ saliva and blood, along with bacteria and, possibly, viruses that might turn out to be interesting. Following a complex set of steps, Anthony isolates all the genetic material within the sample. Then he embarks on a hunt, using tiny bits of genetic code—the technical term is “primer”—that match with and bind to specific points in a virus’s unique sequence. You can think of it as a fishing expedition, except the bait is something like a piece of Velcro. Instead of hooks and loops, the Velcro has the nucleotides that make up DNA: adenine, cytosine, guanine and thymine.
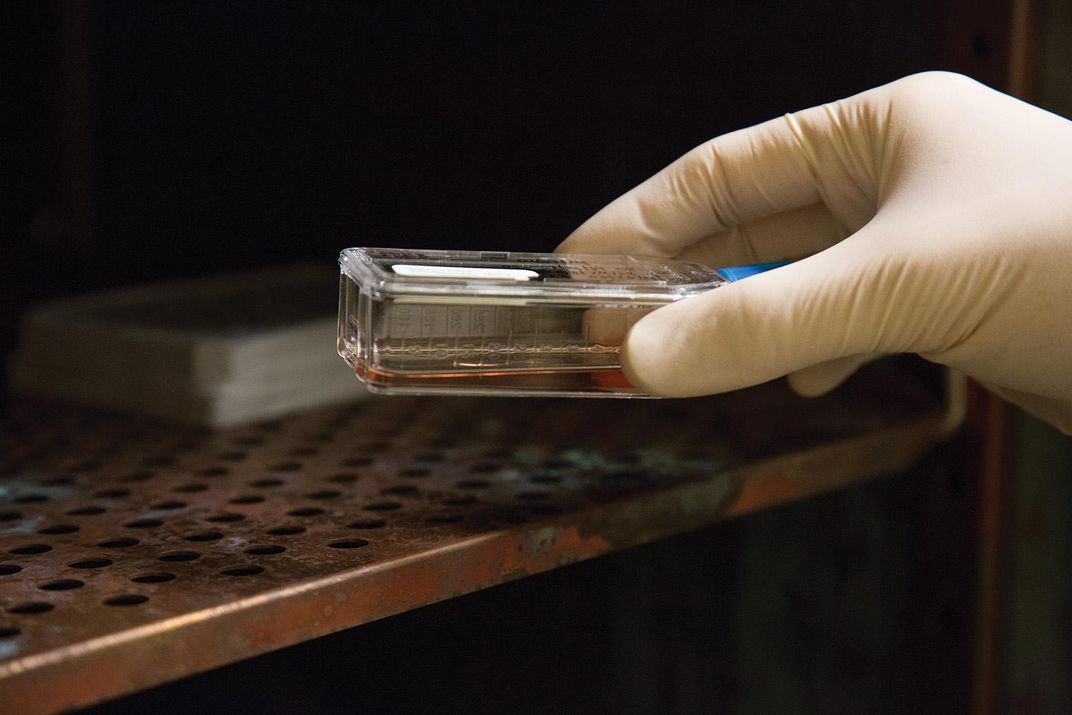
That method—called polymerase chain reaction—is a cheap and simple way to do a broad sweep for viruses, but it brings up limited information. Once Anthony finds that a sample has a virus in it, he tests it with another, more complicated process called deep sequencing. This generates millions of fragments of genetic material from everything in the sample. The challenge is to fish out all the sequences that belong to the virus he wants to study and stitch them all together. A computer does this by comparing the nucleotide sequences in the recovered bits with the sequences of known viruses. “We put it together like a puzzle,” says Anthony. “You have all of this data, all these millions and millions of sequences, and you have to find the little pieces and stitch them together.” On his monitor, the process looks like building a wall of tiny Legos.
Once a sequence is assembled, Anthony can compare it to other viruses using what are known as phylogenetic trees—they look like family trees laid out horizontally, showing the evolutionary relationships. These trees can help scientists spot patterns. For instance, do two closely related viruses come from the same part of the world? Or from the same type of bat?
Multiply that process by the thousands of samples Predict has collected, and the data set transforms into an early warning system, a pointer to hot spots and species where pandemic pathogens might emerge. “If you wait until a virus is killing people,” says Suzan Murray, a wildlife veterinarian who is the program director of the Smithsonian’s Global Health Program, “and then try to figure out what kind of virus it is, sequence it, backtrack to figure out what the host might be and then what people might be doing to put themselves in harm’s way, you’ll lose hundreds of thousands of human lives, and billions, trillions of dollars.” That, of course, is just what the Covid-19 pandemic has done.

Anthony was involved in work that established bats as major reservoirs for coronaviruses; identified hot spots of SARS-like viruses in Africa and Southeast Asia; and identified a previously unknown coronavirus, found in a bat, that closely resembles the MERS virus but lacks a genetic adaptation that would allow it to spread to humans. The group found potentially new adenoviruses in rodents in the Democratic Republic of Congo; herpes viruses in macaques in Malaysia; and a novel ebolavirus in bats in Sierra Leone. Piece by piece, over ten years, Predict researchers and partners in the U.S. and abroad had started assembling an atlas of risks to humanity—949 newly identified viruses, and 217 known ones found in species they had not been associated with—while also mapping the behaviors that made humans vulnerable.
In April, researchers at Smithsonian’s National Zoo published a paper announcing the discovery of six new coronaviruses from bats in Myanmar. The paper was written in 2019 but came out just as the current Covid-19 pandemic was shutting down schools and businesses around the world.
By that time, the Predict project itself was in the midst of being shut down.
* * *
Now that the novel coronavirus has demonstrated how much havoc a zoonotic pathogen can create, the value of tracking down viruses before they leap from the animal world might seem obvious. But Predict, and the whole enterprise of calculating which pathogens pose the most risk, is still surprisingly controversial. The criticism, in brief: It’s one thing to identify potentially zoonotic pathogens and the animals that carry them. It’s a much larger task—and so far, not achieved—to pinpoint which of them will cause a human epidemic.
“There is no simple algorithm that will enable an accurate prediction of what viruses might emerge in the future,” Jemma L. Geoghegan of Macquarie University and Edward C. Holmes of the University of Sydney wrote in 2017 in the journal Open Biology. “It is necessary to lower our expectations about disease emergence as a predictive science.”
In 2018, Holmes, Andrew Rambaut of the University of Edinburgh and Kristian G. Andersen of the Scripps Research Institute in California argued in the journal Nature: “Broad genomic surveys of animal viruses will almost certainly advance our understanding of virus diversity and evolution. In our view, they will be of little practical value when it comes to understanding and mitigating the emergence of disease.”

Even as recently as March, when the novel coronavirus was already spreading, Colin J. Carlson of Georgetown University’s Center for Global Health Science and Security, said in The Lancet Microbe: “Our field, as currently positioned, is still not ready to stop current or future pandemics.”
These critics argue that there are just too many viruses. By one estimate, 1.6 million animal viruses are yet to be discovered in mammal and bird populations, and there’s currently no way to zero in on the estimated 827,000 of them that could cause disease in humans. Geoghegan and Holmes point out that Zika virus was identified in 1947, yet this 68-year head start didn’t keep it from causing an epidemic in 2015. Some scientists argue that the federal funding used for Predict would have been better spent on shoring up public health protections, such as vaccines and antiviral drugs.
“Predict did important work in basic science with viral sampling and surveillance at the human-animal interface,” says Caitlin Rivers, an assistant professor at the Johns Hopkins Center for Health Security who in February criticized the program on Twitter. “But it’s not clear to me how you get from that activity to actually predicting and interrupting pandemics.”
The people within Predict counter that even though they didn’t pinpoint the virus that causes Covid-19, the work they did showed that bats are the most important hosts of coronaviruses, and that viruses closely related to this one come from Rhinolophus and Hipposideros bats. This information will make it easier to figure out where other SARS-like viruses might be circulating. Lab staff in Thailand and Nepal whom Predict had trained also helped identify the first cases in their countries, in travelers from China.

Under USAID, Predict was on a five-year grant cycle. At its founding in 2009, it got five years of funds, guaranteeing its survival into 2014. In 2014, it got five more years, which funded it through September 2019. That funding was up for renewal in fall 2019. Instead, it was extended for just six more months, through March 2020.
Carroll, who left USAID after the recent nonrenewal, says he doesn’t think that decision was explicitly political. “It was a bureaucratic response, never elevated to the White House level,” he said. But White House budget plans had already proposed cutting funds to the section of USAID that granted Predict’s money, the Bureau for Global Health. It was part of the current administration’s broader pattern of backing away both from international agreements and public health defenses: It had already disbanded the National Security Council’s Directorate for Global Health Security and Biodefense, known informally as the “pandemic response unit,” and proposed cuts in the global-health divisions of the Centers for Disease Control and Prevention and the Department of Homeland Security.
In March, Predict prepared to wind down, holding its final meeting over Zoom. By that point, the novel coronavirus was transmitting around the world. It had reached every habitable continent before the end of February, and on April 2, passed one million cases worldwide.
What had not been explicitly political suddenly became so. Senator Elizabeth Warren of Massachusetts, while still a presidential candidate back in January, had put forward a plan for countering infectious disease threats that included refunding Predict. On March 5, she and Senator Angus King of Maine demanded that USAID explain the cancellation to Congress. The attention won Predict a reprieve: an additional $2.26 million that will let the project continue until the end of September.
On May 1, USAID posted a “notice of funding opportunity” for a Predict successor—a $100 million project called Strategies to Prevent (STOP) Spillover. The new project will also work with targeted countries to prevent viruses from jumping from wild to human worlds. But unlike Predict, STOP Spillover plans to address viruses that scientists already know are out there. It isn’t looking for new organisms ready to make the leap.
Meanwhile, the virus behind Covid-19 became the center of conspiracy theories, some of them promoted by political leaders. These theories contended that the virus was not part of a natural spillover, but a bioweapon created in a Chinese lab. On April 30, the U.S. Office of the Director of National Intelligence tried to put the matter to rest: “The entire Intelligence Community...concurs with the wide scientific consensus that the Covid-19 virus was not manmade or genetically modified.” Still, politicians continued to express suspicion toward scientists in Wuhan, China, where the pandemic originated.
This had repercussions for the EcoHealth Alliance, one of the Predict partners. At the end of April, the National Institutes of Health canceled a longstanding, peer-reviewed $3.7 million grant to the EcoHealth Alliance because it had sent $76,000 of the grant money to the Wuhan Institute of Virology to support joint work on bat coronaviruses. The cancellation came after a reporter mischaracterized the grant in a question to President Trump, and it sparked a furious reaction, including letters of protest sent to the National Institutes of Health. One of these letters was signed by 77 Nobel laureates, and another came from the membership of 31 scientific societies, totaling several hundred thousand scientists.
Meanwhile, Carroll is moving on. In February, he incorporated a new nonprofit called the Global Virome Project. The project is still in its infancy and seeking out funding, but it aims to massively scale up the work of Predict, recruiting national laboratories across the globe. The goal is to create a shared atlas and surveillance network for the still-unidentified viruses believed to exist in mammals and birds.
“It’s about changing the paradigm,” Carroll says. “From waiting and reacting, to going where the viruses are, before they come to us.”
* * *
In the meantime, the risks of new virus spillovers are not decreasing. “These things are out there, waiting to emerge, and we’re doing everything possible to help them emerge,” says Peter Daszak, a disease ecologist who is the EcoHealth Alliance’s president. “We’re going into bat caves, sheltering from the rain. We’re digging out bat feces, spreading it on vegetable plots across Southeast Asia, selling it online as medicine. We’re hunting bats to take them home, and chop them up and eat them or sell them, getting bitten, getting scratched. That’s happening millions of times a year. And we’re connected to where that happens by less than a day’s travel. It’s just the perfect storm.”

Throughout the early months of the pandemic, Anthony kept going to work. Part of his role at Columbia is to manage the secure laboratory where viruses can be analyzed without posing a hazard, and that was considered essential. As he walked through the emptied city, he thought about the lessons posed by the many viruses he has examined. “It’s critically important that we try to identify where this virus came from, so that we can have some idea whether this will happen again,” he says.
Last summer, Anthony and his partner, Andrew, bought an English setter puppy, a reminder of Anthony’s home that they named Argus, after a creature in Greek mythology that could see in every direction because it was covered with 100 eyes. Being an English setter, Argus the dog is covered in spots. (“I wish I had the seeing power of Argus when it comes to predicting emerging infectious diseases,” Anthony says.) In the evenings after Anthony left the lab, scientist and dog would walk the empty streets together. Argus trotted dutifully on a leash at his heels, but every time they passed a fenced dog park, locked to keep people from congregating unsafely, Anthony could feel the puppy yearning for freedom.
He shares the dog’s longing for things to return to normal. But he hopes, when that comes, that we don’t lose the insight we have painfully gained.
“I hope it is a wake-up call,” he tells me. “We have to be more prepared. We have to understand this risk better.” When the current pandemic is contained, it will be essential to remember how quickly the entire world can be shut down by a single virus—and how everyone’s lives can change.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/f9/3f/f93f316c-a803-458c-ad82-c2d589667fcb/virus_hunters_mobile.jpg)
:focal(1247x400:1248x401)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/33/27/33276611-704a-4814-ad44-02c927bcb3a2/desktop_opener_-_blk_v4.jpg)