Should We Destroy Our Last Living Samples of the Virus That Causes Smallpox?
Later this month, the World Health Organization will decide whether or not to get rid of two live virus repositories in the United States and Russia
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/83/d8/83d833b3-8903-46c5-8b5e-a6746394b57f/42-57306747edit.jpg)
Smallpox was perhaps one of the most dangerous diseases on Earth. One variant of the disease has a 30% fatality rate; in Europe smallpox is believed to have claimed around 400,000 lives per year by the end of the 18th century, and worldwide an estimated 300 million people died of smallpox in the 20th century alone. The disease has gruesome physical symptoms—welts filled with opaque fluid that ooze and crust over, leaving survivors scarred with the remnants of its hallmark skin lesions and bumps.
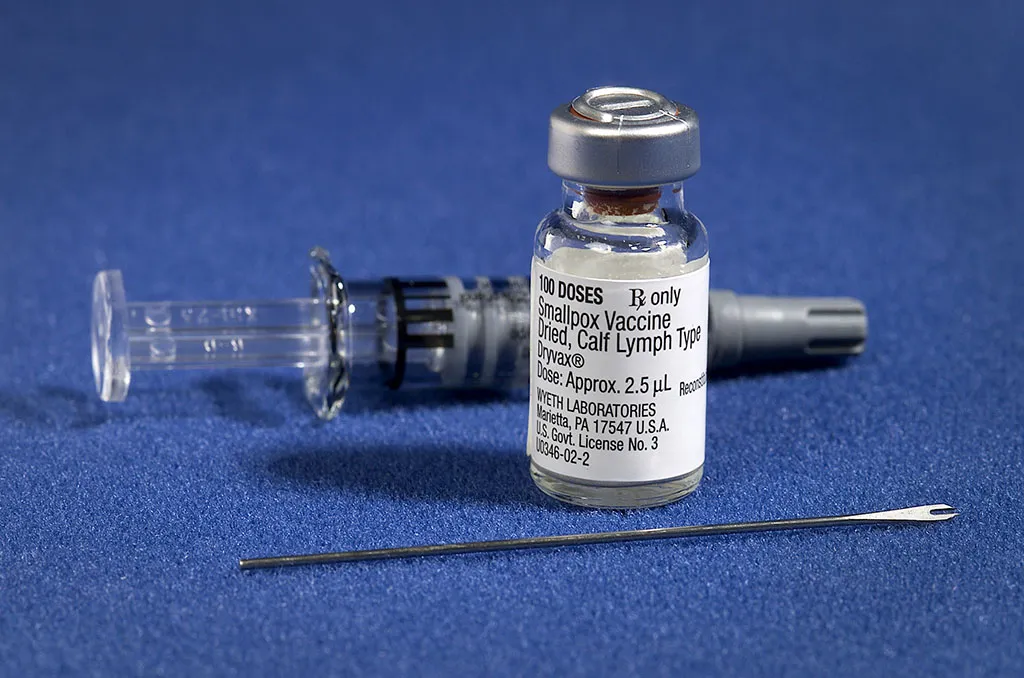
This month the World Health Organization (WHO) will meet to decide whether or not to destroy the last living strains of the variola virus, which causes smallpox. Since the WHO declared the disease eradicated in 1979, the scientific community has debated whether or not to destroy live virus samples, which have been consolidated to laboratories in Russia and at the U. S. Centers for Disease Control and Prevention (CDC) in Atlanta. Small frozen test tubes preserve the surviving strains, and most were collected around the time of eradication, though some date to the early 1930s.
Inger Damon, who leads the poxvirus and rabies branch at the CDC, and her colleagues argue in an editorial in PLoS Pathogens today to save the virus from full extinction. According to Damon, retaining the live samples will allow researchers to delve into unanswered questions about the variola virus and to test better vaccines, diagnostics, and drugs. “There is more work to be done before the international community can be confident that it possesses sufficient protection against any future smallpox threats,” they write.

She notes that the live virus has already been used to find compounds that naturally fight smallpox and to test vaccine candidates with fewer side effects, like IMVAMUNE. “If we don’t have the virus, we won’t be able to test some of these compounds or test serum from vaccines again the virus itself,” says Damon.
But do we really need all of these vaccines for a disease that’s no longer around in humans? The last natural case was diagnosed in 1977, and today, the risk of a smallpox outbreak emerging is minuscule. However, scientists don’t know exactly how long variola virus can survive in dead tissue.
Researchers have successfully revived ancient viruses when the right environmental conditions preserve a specimen. Thus, live forms of the virus could potentially come from frozen mummies and old tissue samples. And when such specimens do turn up, they raise valid alarms: New York construction workers unearthed a 19th-century woman who died of smallpox in 2011 and immediately called in the CDC, only to find that her corpse didn’t pose a threat to humans. A smallpox scab preserved in a letter from 1876, recently on display at a museum in Virginia, raised a scare, but turned out to be harmless.
So, Damon argues, it’s perhaps better to be safe than sorry. Plus, vaccines and medications tested against variola virus could prove useful in other poxviruses—smallpox relatives do keep popping up.
Using the live samples of the virus, researchers have delved into its evolutionary genetics and learned that smallpox is between 8,000 and tens of thousands years old. Part of what makes smallpox so interesting to researchers is the fact that it only infects humans, but likely jumped from an animal host to humans thousands of years ago.
“Trying to understand what is unique about this virus has always been an interesting scientific question,” says Damon, who thinks there are still gaps in knowledge about smallpox evolution and how the virus interacts with the human immune system.
But not everyone thinks that having the live virus around is absolutely vital to achieve these research goals. “I don’t agree that more is left to be done that cannot be done without live variola virus,” says Gregory Poland, an immunologist who develops vaccines at the Mayo Clinic in Minnesota. Researchers could test vaccines and drugs against smallpox relatives like monkeypox and vaccinia—the cowpox strain originally used to develop the smallpox vaccine, he says. He points out that fragments of the smallpox genome have been sequenced, and researchers could string these together to synthesize an approximate variola genome.
Unfortunately, the same know-how and scientific technology could allow bioterrorist to turn smallpox into a weapon. “The progress that’s been made in synthetic biology over the past five years is pretty phenomenal, so I think it raises the specter that there’s a greater possibility that someone could attempt this,” says Damon. It's possible that some strains also slipped through the cracks or were hidden when samples were consolidated, too.
Though the risk of someone using smallpox as a weapon might seem far-fetched, if history is any indication a synthetic version could do a lot of damage. But, the U. S. has been stockpiling anti-viral drugs in the event that a smallpox bio-attack becomes a reality. Would it still, then, be important to have samples of the variola virus?
Poland thinks not, because most public health facilities around the world have the means to isolate, treat, and vaccinate patients. But Damon points out that having a live virus around would allow scientists to quickly make sure new drugs, vaccines, and diagnostics are working the way they’re supposed to in the face of such a threat.
The WHO has been at this crossroads before, and the same players brought up similar scientific and political quandaries. For example, when the WHO last debated the issue in 2011, Poland argued that just having the live virus might create the false perception that the U. S. might be using it to develop biological weapons. Maintaining the samples comes with a risk of accidental release, as with any other high-risk pathogen.
To Poland, those risks are ultimately unnecessary; in fact, he argues that we have an ethical burden to destroy the virus or at least restrict its research use and access. “An accidental release, no matter how small the risk is an unacceptable risk, given the lack of any possible utility in keeping the virus,” he said in 2011.
So, do we keep the variola virus around for research or doom it to death by autoclave, a device that generates extreme temperatures and pressures to sterilize biological samples?
The WHO will open their discussion later in May. They have the option to decide the fate of the viral samples or defer—an option they’ve chosen every time the issue comes up. So, it’s more than likely that the world’s last smallpox samples will live to see another biosafety lab freezer and that the debate will go on.
What would you do—keep or destroy the virus? Let us know your thoughts.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Screen_Shot_2014-01-27_at_12.05.16_PM.png)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Screen_Shot_2014-01-27_at_12.05.16_PM.png)